Phosphorus is a critical electrolyte that supports energy production, muscle contraction, oxygen delivery, and cellular function. In malnourished patients, phosphorus imbalance—especially hypophosphatemia—can quickly become life-threatening. Every nurse, registered nurse, and RN nurse must recognize this risk early to provide safe, effective nursing care and to succeed on the NCLEX.
This guide explains why phosphorus drops in malnutrition, how it affects the body, and what nursing actions prevent serious complications. It is ideal for inclusion in any nursing bundle focused on electrolytes or nutrition.
🔍 Why Phosphorus Is Important
Phosphorus plays a key role in:
- ATP (energy) production
- Muscle and diaphragmatic contraction
- Red blood cell oxygen release
- Acid–base balance
- Bone strength
Without enough phosphorus, cells cannot generate energy, leading to systemic failure.
🧪 Normal Phosphorus Levels
- 2.5–4.5 mg/dL
Even mild decreases can cause significant neuromuscular and respiratory effects in malnourished patients.
🔻 Hypophosphatemia in Malnourished Patients (Most Common)
Why It Happens
Malnourished patients often develop hypophosphatemia due to:
- Inadequate dietary intake
- Chronic alcoholism
- Anorexia nervosa
- Prolonged fasting or starvation
- Malabsorption syndromes
However, the greatest risk occurs during refeeding syndrome.
⚠️ Refeeding Syndrome: Critical NCLEX Concept
When nutrition is restarted:
- Insulin release increases
- Phosphorus shifts into cells
- Serum phosphorus drops rapidly
This sudden shift can cause severe hypophosphatemia within 24–72 hours.
🩺 Nursing Assessment: Signs of Low Phosphorus
A registered nurse should assess for:
Neuromuscular Symptoms
- Muscle weakness
- Paresthesia
- Decreased reflexes
- Confusion
Respiratory Symptoms
- Shallow breathing
- Respiratory muscle weakness
- Difficulty weaning from ventilator
Cardiac Symptoms
- Decreased contractility
- Arrhythmias
- Hypotension
These findings may appear suddenly and worsen quickly.
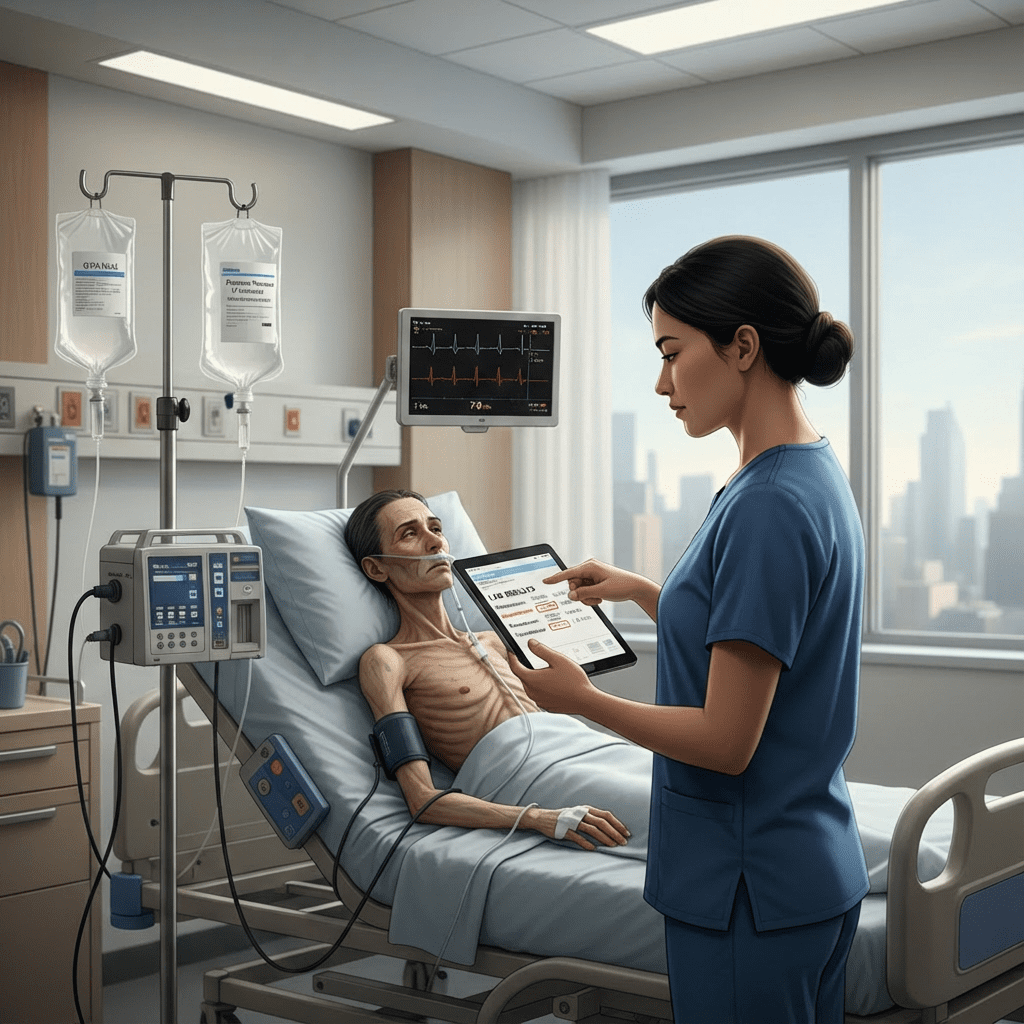
👩⚕️ Nursing Interventions for Hypophosphatemia
An RN nurse should:
- Monitor phosphorus levels closely during refeeding
- Initiate cardiac and respiratory monitoring
- Administer phosphate replacement as prescribed
- Start nutrition slowly and gradually
- Monitor calcium and magnesium levels
- Assess muscle strength and respiratory effort
⚠️ Rapid phosphate replacement can cause hypocalcemia, so careful monitoring is essential.
🔺 Hyperphosphatemia in Malnourished Patients (Less Common)
Although less common, hyperphosphatemia can occur, especially in patients with renal failure.
Possible Causes
- Impaired renal excretion
- Excess phosphate supplementation
- Tumor lysis syndrome
🩺 Nursing Assessment: High Phosphorus
- Muscle cramps
- Tetany
- Itching
- Hypocalcemia symptoms
👩⚕️ Nursing Interventions for Hyperphosphatemia
- Restrict dietary phosphate
- Administer phosphate binders
- Monitor calcium levels
- Assess renal function
- Encourage adequate hydration if appropriate
🔄 Relationship Between Phosphorus and Other Electrolytes
Phosphorus imbalance often affects:
- Calcium (inverse relationship)
- Magnesium
- Potassium
Correcting phosphorus may require addressing multiple electrolytes—an important NCLEX concept.
🧠 NCLEX Tips for Phosphorus Imbalance
- Malnourished patients are at highest risk for hypophosphatemia
- Refeeding syndrome causes rapid phosphate shifts
- Muscle weakness + difficulty breathing = suspect low phosphorus
- Always start nutrition slowly
- Monitor electrolytes frequently during refeeding
🩺 Why Nurses Must Monitor Phosphorus Closely
Untreated hypophosphatemia can lead to:
- Respiratory failure
- Cardiac dysfunction
- Rhabdomyolysis
- Hemolysis
- Death
A proactive nursing approach prevents complications and improves outcomes.
✅ Key Takeaways
- Hypophosphatemia is common in malnourished patients
- Refeeding syndrome is a major risk
- Phosphorus is essential for energy and muscle function
- Respiratory assessment is a nursing priority
- Electrolytes must be corrected gradually
🏁 Final Thoughts
Understanding phosphorus imbalance allows nurses to protect vulnerable malnourished patients during nutritional recovery. Whether studying for the NCLEX or practicing bedside nursing, this knowledge is essential for every registered nurse and RN nurse.
❓ FAQ
Malnourished patients have depleted phosphorus stores due to poor intake. When nutrition is restarted, insulin causes phosphorus to shift into cells, lowering serum levels rapidly.
Respiratory failure. Phosphorus is essential for ATP production, and low levels weaken the diaphragm and respiratory muscles.
Refeeding syndrome is a metabolic disturbance that occurs when nutrition is reintroduced too quickly, causing electrolyte shifts—especially low phosphorus.
Slow initiation of nutrition and close electrolyte monitoring, especially phosphorus, potassium, and magnesium.