Potassium balance plays a life-saving role during diabetic emergencies. Conditions such as diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS) cause dramatic potassium shifts that can quickly lead to fatal cardiac arrhythmias. For this reason, every nurse, registered nurse, and RN nurse must understand how potassium behaves in these emergencies to provide safe, effective nursing care and succeed on the NCLEX.
This article breaks down potassium physiology, lab interpretation, and nursing interventions in a clear, step-by-step format suitable for any nursing bundle or exam review.
🔬 Why Potassium Shifts Occur in Diabetic Emergencies
In diabetic emergencies, insulin deficiency and acidosis push potassium out of the cells and into the bloodstream. Although lab values may initially appear normal or elevated, the total body potassium is actually depleted due to osmotic diuresis and vomiting.
This concept is critical for NCLEX success and real-world patient safety.
🧠 Key Concept for Nurses
Serum potassium does NOT reflect total body potassium in DKA or HHS.
A registered nurse must anticipate dangerous potassium drops once insulin therapy begins.
⚠️ Potassium in Diabetic Ketoacidosis (DKA)
Initial Potassium Status
- Serum potassium may be normal or high
- Total body potassium is low
Why This Happens
- Insulin deficiency causes potassium to leave cells
- Acidosis shifts potassium into serum
- Urinary potassium loss continues due to osmotic diuresis
🩺 Nursing Assessment in DKA
An RN nurse should closely monitor:
- Serum potassium levels
- ECG changes (peaked T waves, flattened T waves)
- Muscle weakness
- Cardiac rhythm
- Urine output
- Acid-base status
💉 Effect of Insulin Therapy on Potassium
Once insulin is administered:
- Potassium shifts back into the cells
- Serum potassium can drop rapidly
- Risk of life-threatening hypokalemia increases
⚠️ NCLEX Priority Rule
Never start insulin if potassium is < 3.3 mEq/L
Potassium replacement must occur first.
🔁 Potassium Replacement Guidelines (Nursing Focus)
| Potassium Level | Nursing Action |
|---|---|
| < 3.3 mEq/L | Hold insulin, give IV potassium |
| 3.3–5.2 mEq/L | Give potassium with IV fluids |
| > 5.2 mEq/L | Do NOT give potassium; monitor closely |
These values are high-yield NCLEX facts.
💧 Potassium in Hyperosmolar Hyperglycemic State (HHS)
Although HHS has little or no ketosis, potassium shifts still occur.
Nursing Considerations
- Severe dehydration causes potassium loss
- Potassium may initially appear normal
- Insulin therapy can still cause hypokalemia
The nursing approach to potassium management in HHS mirrors that of DKA.
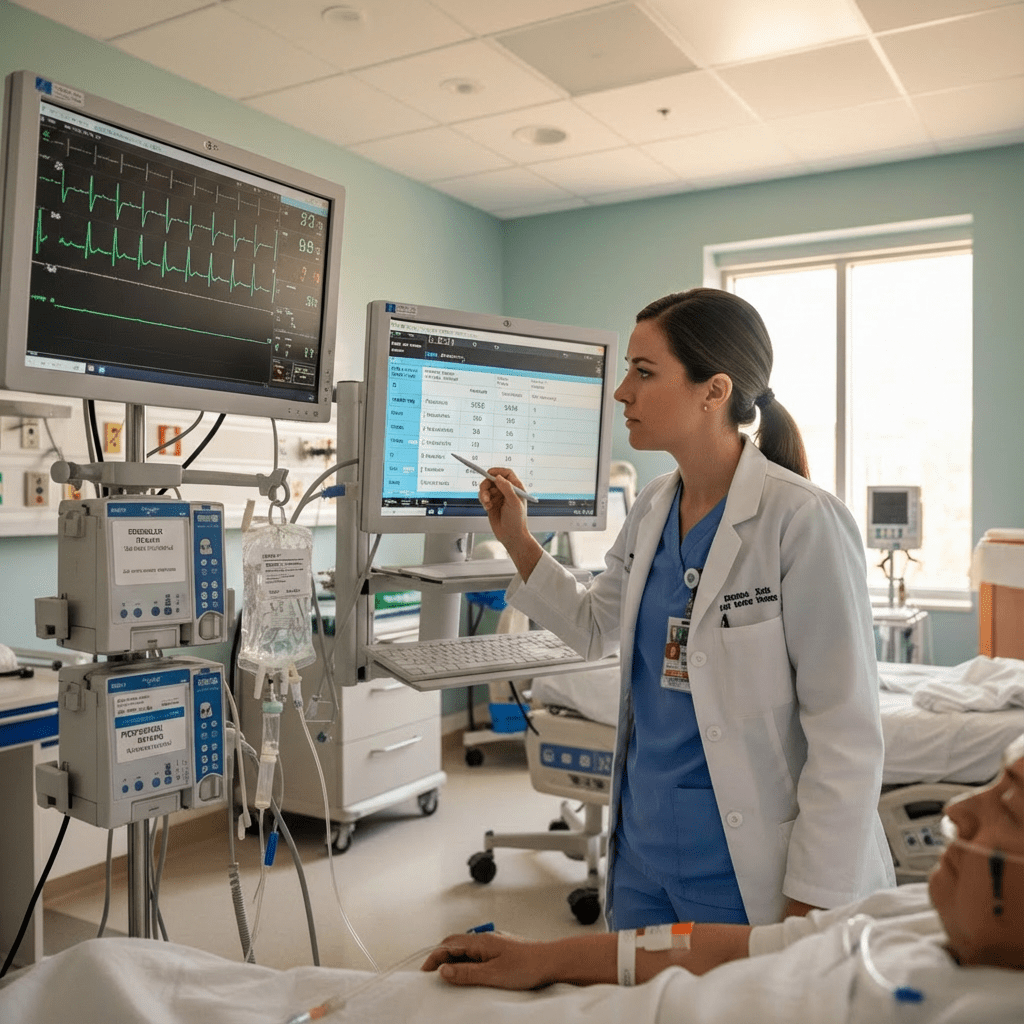
🩺 Cardiac Monitoring: RN Nurse Priority
Potassium imbalances directly affect the heart. A registered nurse should:
- Place the patient on continuous ECG monitoring
- Watch for dysrhythmias
- Monitor QT interval changes
- Recognize early signs of cardiac instability
Both hyperkalemia and hypokalemia can cause sudden cardiac arrest.
🧠 NCLEX Tips for Potassium in Diabetic Emergencies
- High potassium on labs does NOT mean excess potassium
- Insulin lowers potassium levels
- Potassium replacement often begins early in treatment
- Cardiac monitoring is mandatory
- Hypokalemia is more dangerous than hyperkalemia during treatment
NCLEX questions often test what to do first — potassium assessment always comes before insulin.
🩺 Patient Safety & Nursing Education
A strong nursing bundle should emphasize:
- Frequent electrolyte monitoring
- IV pump accuracy
- Clear documentation of lab trends
- Patient education about insulin adherence
- Early recognition of dehydration symptoms
Education reduces recurrence and improves long-term outcomes.
✅ Key Takeaways for Nurses
- Total body potassium is depleted in DKA and HHS
- Serum potassium may appear misleading
- Insulin therapy shifts potassium intracellularly
- Hypokalemia is the biggest immediate risk
- Every RN nurse must monitor ECG and labs closely
🏁 Final Thoughts
Understanding potassium shifts in diabetic emergencies allows nurses to prevent fatal complications and deliver safe, evidence-based care. Whether you’re preparing for the NCLEX, working bedside, or building a comprehensive nursing bundle, mastering this topic is essential for every registered nurse.
❓ FAQ
In diabetic emergencies, lack of insulin and acidosis force potassium out of cells into the blood. Although lab values may look normal or high, total body potassium is actually depleted.
Once insulin therapy begins, potassium shifts back into cells rapidly. This can cause dangerous hypokalemia, leading to life-threatening cardiac arrhythmias.
If potassium is below 3.3 mEq/L, insulin must be held. A registered nurse should initiate potassium replacement first. This is a high-yield NCLEX rule.
Both high and low potassium levels can trigger arrhythmias. Continuous ECG monitoring allows the RN nurse to detect early cardiac instability.