The postpartum period is a vulnerable time when new mothers face a higher risk of infection due to physiological changes, open wounds after childbirth, and exposure to hospital pathogens. For every registered nurse (RN nurse) and student preparing for the NCLEX, mastering postpartum infection prevention is essential for safe maternal care. This guide simplifies what every nurse should know and what you can teach families to support healing at home.
Why Infection Prevention Matters in Postpartum Care
After delivery—whether vaginal or cesarean—the mother’s body experiences major changes. The uterus undergoes involution, the perineum may have lacerations, and the cesarean incision becomes an open surgical site. Because of these factors, postpartum patients are at risk for:
- Endometritis
- Urinary tract infections
- Mastitis
- Wound infections
- Respiratory infections after anesthesia
Early identification and prevention are critical nursing responsibilities. For the NCLEX, remember that postpartum infection can quickly progress to sepsis, making prevention a high-priority nursing action.
Common Risk Factors Every RN Nurse Should Know
Nursing students often encounter questions about risk factors for postpartum infection, especially in NCLEX scenarios. Key risks include:
- Prolonged labor or ruptured membranes
- Multiple vaginal examinations
- Cesarean birth
- Poor hand hygiene
- Diabetes or anemia
- Retained placental fragments
- Use of a urinary catheter
Understanding these risks helps registered nurses create effective care plans that reduce complications.
Nursing Assessment: Early Signs of Postpartum Infection
When performing postpartum checks, the nurse must watch for red flags. Symptoms include:
- Fever above 38°C (100.4°F)
- Foul-smelling lochia
- Increased uterine tenderness
- Redness, swelling, or discharge from an incision
- Painful, cracked nipples
- Dysuria or urgency
- Fatigue or malaise
A strong assessment skillset is essential in real practice and heavily tested on the NCLEX.
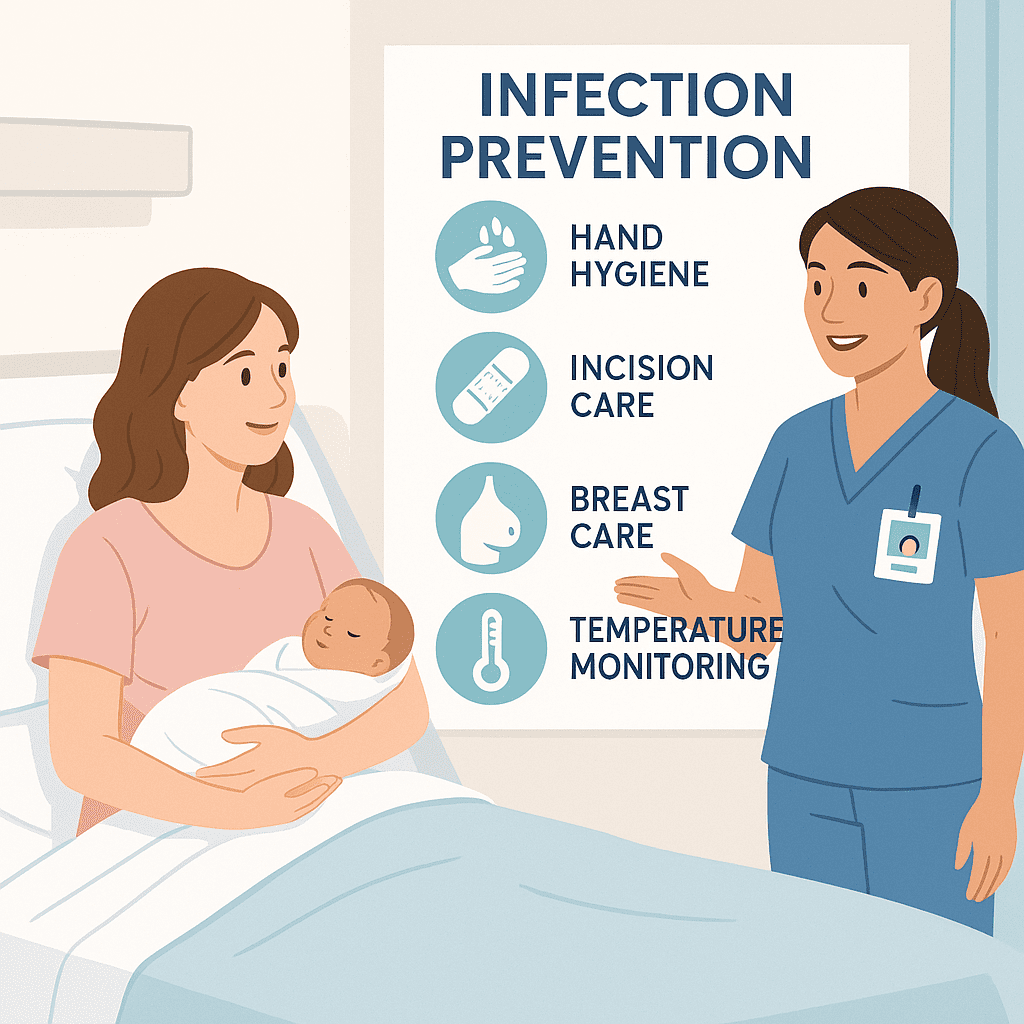
Core Infection Prevention Interventions (Nursing Focus)
1. Strict Hand Hygiene
Handwashing is the most effective infection-control strategy. Nurses should demonstrate proper hand hygiene and reinforce the practice for parents and visitors.
2. Perineal Care Teaching
For mothers who had a vaginal birth, teach:
- Use a peri bottle after each void
- Pat dry instead of wiping
- Change pads frequently
- Avoid tampons or douching
These simple steps dramatically reduce the risk of endometritis.
3. Cesarean Incision Care
RN nurses should instruct patients to:
- Keep the incision clean and dry
- Inspect daily for redness or drainage
- Avoid heavy lifting
- Wear loose, breathable clothes
This education is a common topic in nursing bundles and postpartum NCLEX questions.
4. Breast Care to Prevent Mastitis
Nurses should guide breastfeeding parents to:
- Maintain a consistent feeding schedule
- Ensure proper latch
- Empty the breasts regularly
- Apply warm compresses if engorged
Engorgement and nipple trauma are major infection gateways.
5. Early Ambulation
Moving soon after delivery improves circulation, reduces respiratory infections, and decreases complications from anesthesia and immobility.
6. Foley Catheter Care
If a catheter is present:
- Maintain a sterile closed system
- Keep the bag below the bladder
- Perform perineal care regularly
UTIs are common postpartum, so nurses must be proactive.
Teaching Parents: What Every Nurse Should Explain Before Discharge
Strong patient education is essential for safe recovery at home. Here’s what a registered nurse should teach every postpartum parent:
- Check temperature daily for the first few days
- Report foul-odor lochia, sudden increase in bleeding, or clots
- Watch for breast redness or flu-like symptoms
- Keep the incision clean and report any unusual drainage
- Know when to seek emergency care, especially for fever or severe pain
Clear communication improves outcomes and is emphasized in the NCLEX maternity section.
NCLEX Tip: Prioritization and Safety
Many NCLEX questions ask which postpartum patient the nurse should assess first. As a rule:
➡️ A postpartum patient with fever, foul-smelling lochia, or incision redness is always a priority.
Remember: Signs of infection = potential progression to sepsis.
How Nursing Bundles Can Help Students Master This Topic
If you’re studying for exams or teaching nursing classes, structured nursing bundles covering postpartum care, infection prevention, and maternity concepts can:
- Organize information
- Provide simplified diagrams
- Reinforce NCLEX-style prioritization
- Include practice questions
- Help RN nurses refresh their skills
Well-designed bundles reduce stress and help students study faster and smarter.
Conclusion
Infection prevention during the postpartum period is a vital responsibility of every nurse and registered nurse (RN nurse). With proper assessment, hygiene practices, education, and follow-up, postpartum infections can be significantly reduced. Understanding these principles not only supports safe patient care but also strengthens preparation for the NCLEX exam.
⭐ FAQ: Infection Prevention During the Postpartum Period
Postpartum infections are commonly caused by bacteria entering the uterus, incision site, or breasts after birth. A registered nurse or RN nurse teaches mothers proper hygiene, wound care, and early warning signs to help reduce risks. These causes are important to understand for NCLEX maternal–newborn exams.
Nurses teach parents to look for fever, foul vaginal discharge, severe abdominal pain, redness or drainage from a C-section incision, burning during urination, and breast redness or swelling. These symptoms require immediate medical attention. This topic appears in many nursing bundle study materials.
A nurse provides guidance on perineal hygiene, proper pad changes, handwashing, and avoiding tampons or intercourse until cleared. For NCLEX-style questions, uterine infection prevention is often a priority nursing action.