Essential Guide for NCLEX & Nursing Practice
The immediate newborn assessment is one of the most critical responsibilities for any nurse, especially those working in labor and delivery, postpartum, or newborn care. For NCLEX test-takers and new graduate Rn nurses, the APGAR score remains a high-yield concept included in nearly every nursing bundle related to maternal and neonatal care.
This article breaks down how registered nurses perform the APGAR assessment, what each component means, and how to interpret the score quickly during those first, essential moments of life.
👶 What Is the APGAR Score?
The APGAR score is a rapid newborn evaluation performed at 1 minute and 5 minutes after birth. It helps the Rn nurse determine how well the baby tolerated labor and how well the newborn is adjusting to life outside the womb.
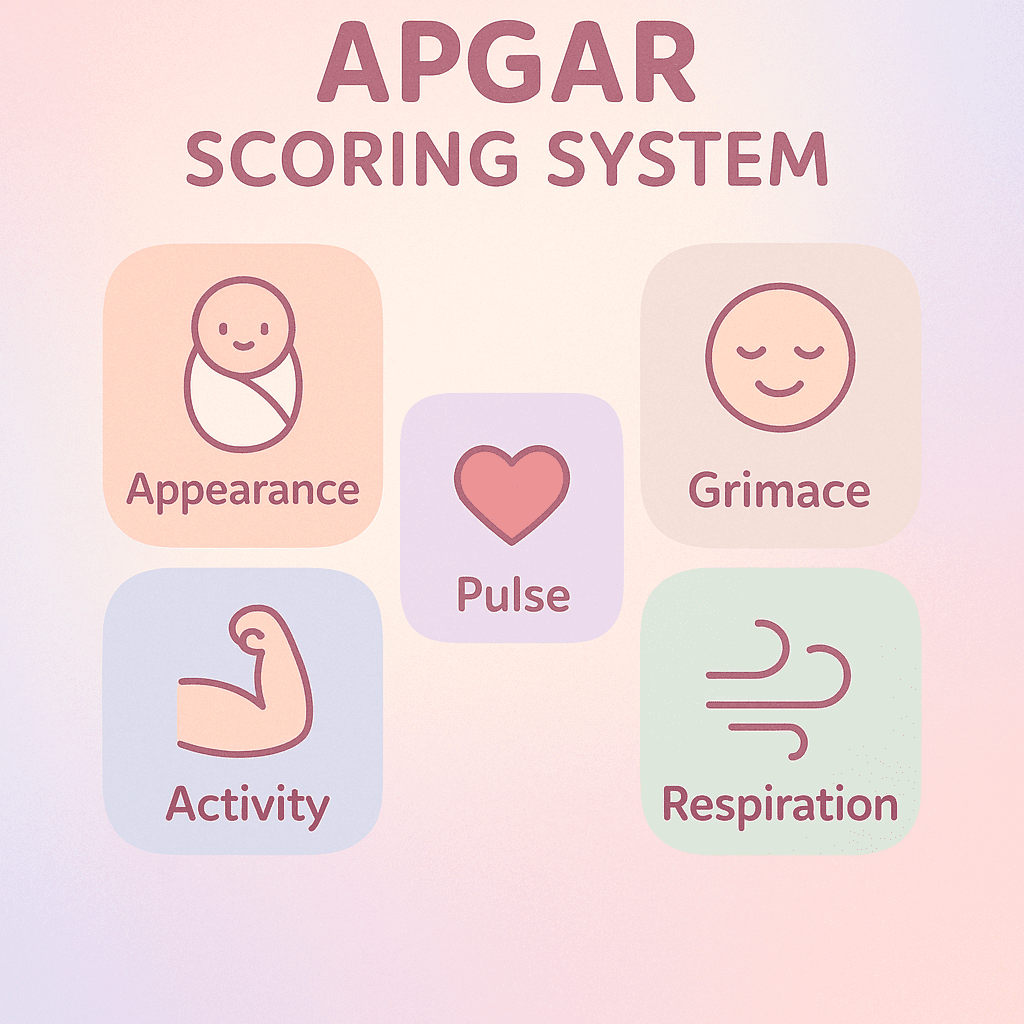
APGAR stands for:
- A — Appearance (Skin Color)
- P — Pulse (Heart Rate)
- G — Grimace (Reflex Irritability)
- A — Activity (Muscle Tone)
- R — Respiratory Effort
Each category scores 0, 1, or 2, with a maximum total of 10.
For NCLEX purposes, remember that the APGAR is NOT used to predict long-term health outcomes. It only evaluates the newborn’s immediate status and whether interventions are needed.
🩺 APGAR Scoring Breakdown for Rn Nurses
Below is a simplified nursing-friendly breakdown—perfect for NCLEX review and bedside practice:
1. Appearance (Skin Color)
- 0 → Blue or pale
- 1 → Pink body, blue extremities (acrocyanosis)
- 2 → Completely pink
🔹 Acrocyanosis is normal for the first few minutes of life and is not a sign of distress.
2. Pulse (Heart Rate)
- 0 → Absent
- 1 → < 100 bpm
- 2 → ≥ 100 bpm
🔹 Heart rate is the most important part of the immediate newborn assessment.
3. Grimace (Reflex Irritability)
- 0 → No response
- 1 → Grimace
- 2 → Cry or active withdrawal
🔹 A strong cry indicates good neurological responsiveness.
4. Activity (Muscle Tone)
- 0 → Limp
- 1 → Some flexion
- 2 → Active movement
🔹 A healthy newborn displays flexed extremities and spontaneous movement.
5. Respiratory Effort
- 0 → Absent
- 1 → Slow or irregular breathing
- 2 → Strong, regular cry
🔹 A vigorous cry indicates effective ventilation.
🧪 How to Interpret APGAR for Nursing Practice
⭐ 7–10 Points: Stable Newborn
- Routine care
- Skin-to-skin
- Monitor temperature, feeding cues
⚠️ 4–6 Points: Moderate Difficulty
- Provide breathing support
- Suction as needed
- Warmth, stimulation, and supplemental oxygen
🚨 0–3 Points: Severe Distress
- Initiate resuscitation immediately
- Positive pressure ventilation
- Notify neonatal team
- Continuous monitoring
For RN nurse candidates preparing for NCLEX, remember:
➡️ A 1-minute APGAR reflects how the baby tolerated birth.
➡️ A 5-minute APGAR evaluates stabilization and adjustment.
🎓 NCLEX Tips for Immediate Newborn Assessment
- The APGAR does not come before resuscitation. If the baby is not breathing, intervene first, then assess.
- Acrocyanosis is normal; central cyanosis is not.
- Heart rate under 100 bpm requires positive pressure ventilation.
- A registered nurse should not delay life-saving interventions simply to assign a score.
- Many NCLEX maternity questions test application, not memorization.
📦 Why This Topic Matters for Your Nursing Bundle
APGAR scoring is included in almost every maternal newborn nursing bundle and is a must-know topic for:
- L&D nurses
- Postpartum nurses
- NICU nurses
- NCLEX candidates
- New RN nurses needing confidence during newborn care
❓ FAQ – Immediate Newborn Assessment (APGAR)
The APGAR score helps the RN nurse quickly evaluate a newborn’s transition to life outside the womb. It guides immediate nursing actions and identifies whether the newborn needs support such as oxygen or resuscitation. On the NCLEX, it is considered an essential early assessment tool.
No. In emergencies, the registered nurse must initiate resuscitation first. The APGAR score is documented afterward. NCLEX questions often highlight that life-saving interventions come before documentation.
A score of 7–10 at 1 and 5 minutes indicates the newborn is adjusting well. The nurse still continues routine newborn nursing care, including temperature regulation, airway support if needed, and bonding.