Abnormal fetal positions can increase the risk of complications during labor and delivery, making early recognition an essential skill for every nurse, especially those preparing for the NCLEX or reviewing maternity content in a nursing bundle. Whether you’re a student, a registered nurse, or an experienced RN nurse, understanding these fetal positions helps ensure safe outcomes for both mother and baby.
What Is an Abnormal Fetal Position?
A fetal position becomes “abnormal” when the baby is not aligned for a smooth vaginal delivery. Normally, the fetus should be in a cephalic, vertex, occiput-anterior position.
When the baby is not in this position, the nurse must quickly assess, anticipate complications, and notify the healthcare provider.
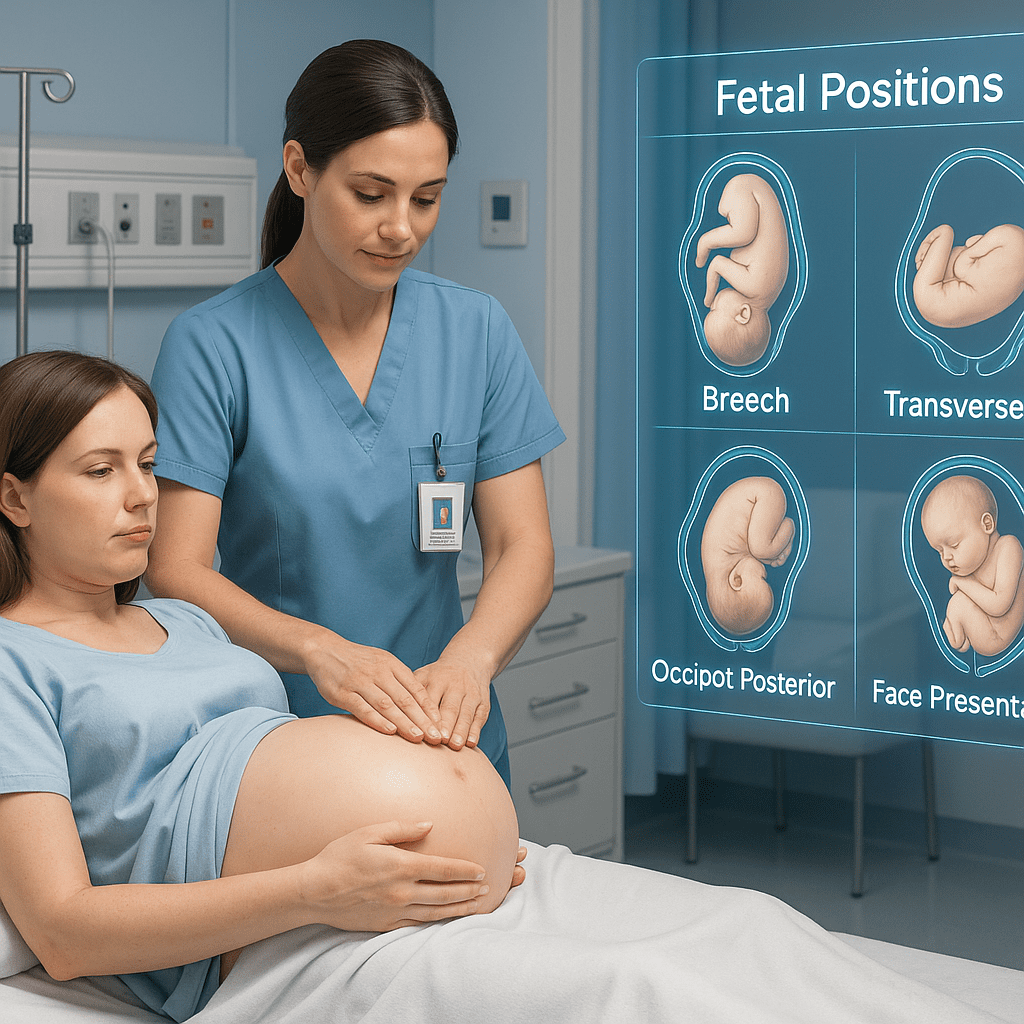
Common Abnormal Fetal Positions and Their Nursing Implications
1. Breech Presentation
The baby’s buttocks or feet present first instead of the head.
Types:
- Frank breech – hips flexed, legs extended
- Complete breech – hips flexed, knees flexed
- Footling breech – one or both feet present first
Nursing Considerations
- Assess fetal heart rate closely.
- Prepare for possible C-section.
- Educate the patient about risks (cord prolapse, birth trauma).
- During the NCLEX, remember breech = higher complication risk.
2. Transverse Lie
The fetus lies horizontally in the uterus.
Why It Matters
Vaginal delivery is not possible.
Nursing Role
- Assist with repositioning attempts (external cephalic version).
- Prepare for C-section if position does not resolve.
- Provide emotional support during labor.
3. Occiput Posterior (OP) Position
The baby is head-down, but facing the mother’s abdomen instead of the spine.
Signs
- Intense back pain (“back labor”)
- Slower dilation
- Irregular contractions
Nursing Interventions
- Encourage hands-and-knees position.
- Use counter-pressure to reduce back pain.
- Reassure the mother—many OP babies rotate during labor.
- NCLEX Tip: OP position increases risk of prolonged labor.
4. Shoulder Presentation
The shoulder is the presenting part.
Nursing Priority
This is an obstetric emergency (risk of cord prolapse).
Interventions
- Do NOT attempt to push the fetus back.
- Immediately notify the provider.
- Prepare for emergency C-section.
5. Face or Brow Presentation
The baby’s face or forehead presents first.
Nursing Considerations
- Assess for fetal distress.
- Prepare for possible operative delivery.
- Monitor closely for molding and trauma.
How Nurses Recognize Abnormal Positions
1. Leopold’s Maneuvers
A fundamental assessment skill for every registered nurse and RN nurse.
Leopold’s helps determine:
- Fetal lie
- Position
- Presentation
- Engagement
2. Vaginal Examination
Can identify the presenting part (head, buttocks, face, shoulder).
3. Fetal Heart Rate Patterns
Abnormal positions may lead to:
- Variable decelerations
- Prolonged labor patterns
- Irregular contractions
4. Ultrasound Confirmation
If the nurse suspects an abnormal position, an ultrasound may be ordered to verify the presentation.
Complications Associated With Abnormal Fetal Positions
- Prolonged labor
- Increased maternal exhaustion
- Cord prolapse
- Shoulder dystocia
- C-section delivery
- Birth injury
These points often appear in NCLEX maternity questions, so understanding them strengthens test performance.
Nursing Role in Managing Abnormal Fetal Position
A nurse plays a critical role in:
1. Early Identification
Using assessment skills and continuous monitoring.
2. Patient Education
Explaining:
- What the fetal position means
- Possible risks
- When a C-section may be needed
3. Intervention
Helping reposition the mother to encourage fetal rotation:
- Hands-and-knees
- Side-lying on the opposite side of fetal back
- Pelvic rocking
- Peanut ball positioning
4. Ensuring Fetal Safety
Monitoring fetal heart rate and reporting abnormalities promptly.
5. Emotional Support
Labor complications can be stressful—nurses provide reassurance and guidance.
Why This Topic Matters for NCLEX and Clinical Practice
The NCLEX frequently tests:
- Fetal presentation recognition
- When to notify the provider
- What interventions the nurse should prioritize
This content is also covered in many nursing bundles and maternity study guides because it is essential knowledge for all maternity nurses.
For registered nurses and RN nurses, recognizing abnormal fetal positions improves maternal–fetal outcomes and enhances clinical confidence.
Conclusion
Understanding abnormal fetal positions is a vital skill every nurse must master. Early recognition and effective intervention can significantly reduce risks during labor. Whether you’re preparing for the NCLEX, improving your maternity knowledge, or reviewing your nursing bundle, mastering fetal positions will strengthen your clinical practice and ensure safer patient care.
❓ FAQ
Any fetal alignment other than cephalic, vertex, and occiput-anterior is considered abnormal. Common examples include breech, transverse lie, and occiput-posterior.
Nurses use Leopold’s maneuvers, fetal heart rate assessment, vaginal exams, and sometimes ultrasound to identify the presentation.
The occiput posterior (OP) position. Mothers often experience intense lower back pain.
Notify the provider immediately—vaginal delivery isn’t possible. Prepare for external cephalic version or C-section.