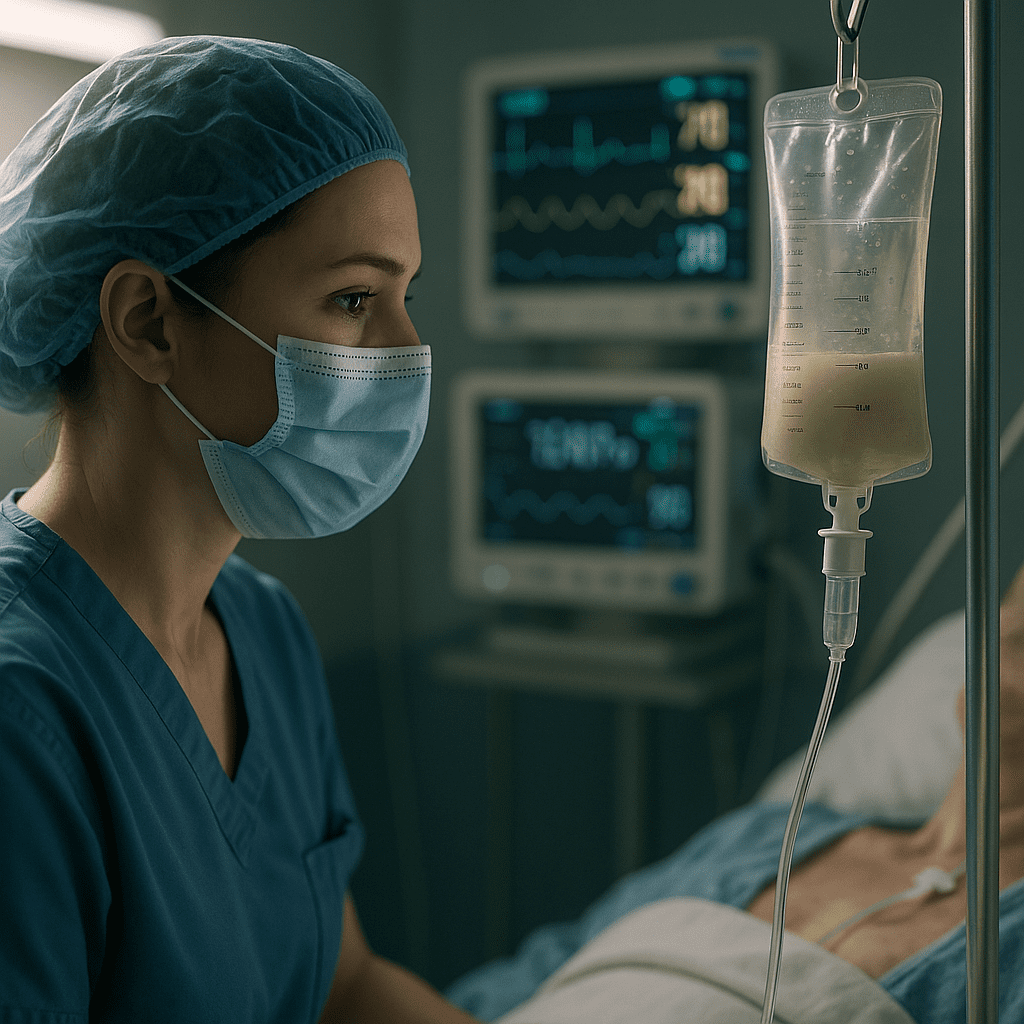
Total Parenteral Nutrition (TPN) is a lifesaving therapy for patients who cannot receive adequate nutrition through the gastrointestinal tract. For every RN nurse and registered nurse, understanding how to monitor TPN is essential for safe and effective patient care—and it’s a high-yield NCLEX topic. TPN management requires strict attention to metabolic changes, fluid balance, infection prevention, and line care. This guide covers everything a nurse needs to know.
⭐ What Is Total Parenteral Nutrition (TPN)?
TPN is a sterile IV solution delivering carbohydrates, fats, proteins, vitamins, electrolytes, and minerals directly into the bloodstream through a central line (PICC, subclavian, or internal jugular). It bypasses the digestive system completely.
It is used for patients with:
- Severe GI disorders
- Crohn’s flare-ups
- Short bowel syndrome
- Severe pancreatitis
- Prolonged NPO status
- Bowel obstruction
For NCLEX, remember:
TPN must be administered through a central line, not a peripheral IV, because of high osmolarity.
🔍 Nursing Responsibilities When Monitoring TPN
Monitoring TPN requires a structured approach. Many nursing bundle resources highlight the same core actions: blood glucose checks, line assessment, electrolyte monitoring, and infection prevention.
✅ 1. Monitor Blood Glucose Closely
TPN delivers concentrated glucose, increasing the risk of hyperglycemia.
The RN nurse should:
- Check blood glucose every 4–6 hours
- Watch for symptoms of hyperglycemia: thirst, polyuria, confusion
- Anticipate sliding-scale insulin orders
NCLEX Reminder:
Never stop TPN abruptly — this may cause rebound hypoglycemia.
✅ 2. Electrolyte Monitoring
TPN can affect potassium, magnesium, phosphate, and sodium levels.
The nurse must review daily labs:
- Potassium (K): Watch for dysrhythmias, muscle weakness
- Phosphate: Risk for refeeding syndrome
- Magnesium: Monitor for tremors or arrhythmias
- Sodium: Assess for confusion, edema
If abnormal values occur, the registered nurse should notify the provider for formula adjustments.
✅ 3. Daily Weight and Intake/Output
A key nursing duty is to track:
- Rapid weight gain → possible fluid overload
- Weight loss → TPN may be insufficient
- Strict intake/output to identify dehydration or overload
NCLEX keyword:
“TPN should maintain steady weight if therapy is effective.”
✅ 4. Central Line Care and Infection Prevention
TPN is a major infection risk because of its high glucose content.
An RN nurse must:
- Use aseptic technique when handling the central line
- Change tubing and filters every 24 hours
- Inspect the site for redness, drainage, or swelling
- Monitor for fever or sepsis signs
Nursing tip:
Never add medications or other fluids to a TPN line.
✅ 5. Monitor for Fluid Overload
Signs include:
- Crackles in lungs
- Edema
- Distended neck veins
- Hypertension
This is especially important in cardiac or renal patients.
✅ 6. Evaluate Patient Response
The nurse should watch for:
- Improved energy
- Weight stabilization
- Wound healing
- Better lab trends
These indicators help determine if the TPN formula is correct.
🛑 Complications Every Nurse Must Know (NCLEX Focus)
✔ Refeeding Syndrome
Occurs when nutrition is restarted after prolonged starvation.
Watch for low phosphate, low potassium, low magnesium.
✔ Infection & Sepsis
Due to central line contamination.
✔ Hyperglycemia/Hypoglycemia
Related to TPN concentration and abrupt interruption.
✔ Fluid overload
Especially in older adults or cardiac patients.
✔ Air Embolism
If tubing or catheter is opened.
📘 Conclusion
Monitoring patients on TPN is a critical responsibility for every nurse and registered nurse. It requires precision, daily assessments, and strict aseptic technique. These principles appear frequently in NCLEX exams and are essential in every clinical setting. Including this information in your nursing bundle helps reinforce safe and evidence-based care for all RN nurses and students.
FAQ: Total Parenteral Nutrition (TPN)
TPN is a method of providing complete nutrition through a central line when a patient cannot use their gastrointestinal tract. It delivers essential nutrients such as carbohydrates, proteins, fats, vitamins, and electrolytes. Every registered nurse (RN) must understand TPN components for NCLEX success and safe patient care.
Monitoring prevents complications such as electrolyte imbalances, hyperglycemia, infection, and fluid overload. A nurse must evaluate daily labs, central line integrity, and patient response. Consistent monitoring is also emphasized in many nursing bundles and NCLEX-style questions.
A RN nurse should assess:
Electrolytes: sodium, potassium, magnesium, phosphate
Liver function tests
Blood glucose
Triglycerides
Typically, every 4–6 hours, especially when initiating therapy. Hyperglycemia is a common complication. Nurses should follow facility protocols and report abnormal values immediately.