Caring for a child with asthma is one of the most important responsibilities for any nurse, especially those preparing for the NCLEX or working as a registered nurse (RN nurse) in pediatric settings. Because childhood asthma is one of the most common chronic conditions worldwide, nursing management requires strong assessment skills, effective communication, and accurate medication administration. Many students use a nursing bundle or pediatric study guide to master these essential concepts.
This article provides clear, simple, and essential information every nurse should know when caring for a child with asthma.
Understanding Childhood Asthma
Asthma is a chronic inflammatory disorder of the airways that leads to:
- Bronchoconstriction
- Airway swelling
- Increased mucus production
For a registered nurse, recognizing these early changes is crucial in preventing severe attacks. Children often present with wheezing, coughing, chest tightness, or difficulty breathing, especially during exercise or illness.
Assessment: What Every RN Nurse Should Look For
Accurate assessment is a major NCLEX priority. A pediatric nurse must evaluate:
1. Respiratory Status
- Respiratory rate
- Use of accessory muscles
- Presence of wheezing
- Breath sounds (diminished = BAD sign)
2. Oxygen Saturation
Maintain O₂ sat > 95% during stable breathing.
3. Level of Distress
- Speaking in short sentences
- Retractions
- Nasal flaring
4. Triggers
Common triggers include smoke, dust, pollen, pets, exercise, and cold air. Teaching families how to avoid these triggers is core nursing practice.
Asthma Medications: What Nurses Need to Know
NCLEX often tests the difference between rescue and controller medications. A well-prepared RN nurse must understand:
1. Short-Acting Beta Agonists (SABA)
Examples: Albuterol
- Rescue inhaler used during acute attacks.
- Teach the child to inhale slowly and deeply.
- Side effects: tachycardia, tremors.
2. Inhaled Corticosteroids (ICS)
Examples: Fluticasone, Budesonide
- Daily controller medication.
- Reduces inflammation and prevents attacks.
- Instruct child to rinse mouth after use to avoid thrush.
3. Leukotriene Modifiers
Example: Montelukast
- Helps reduce nighttime symptoms.
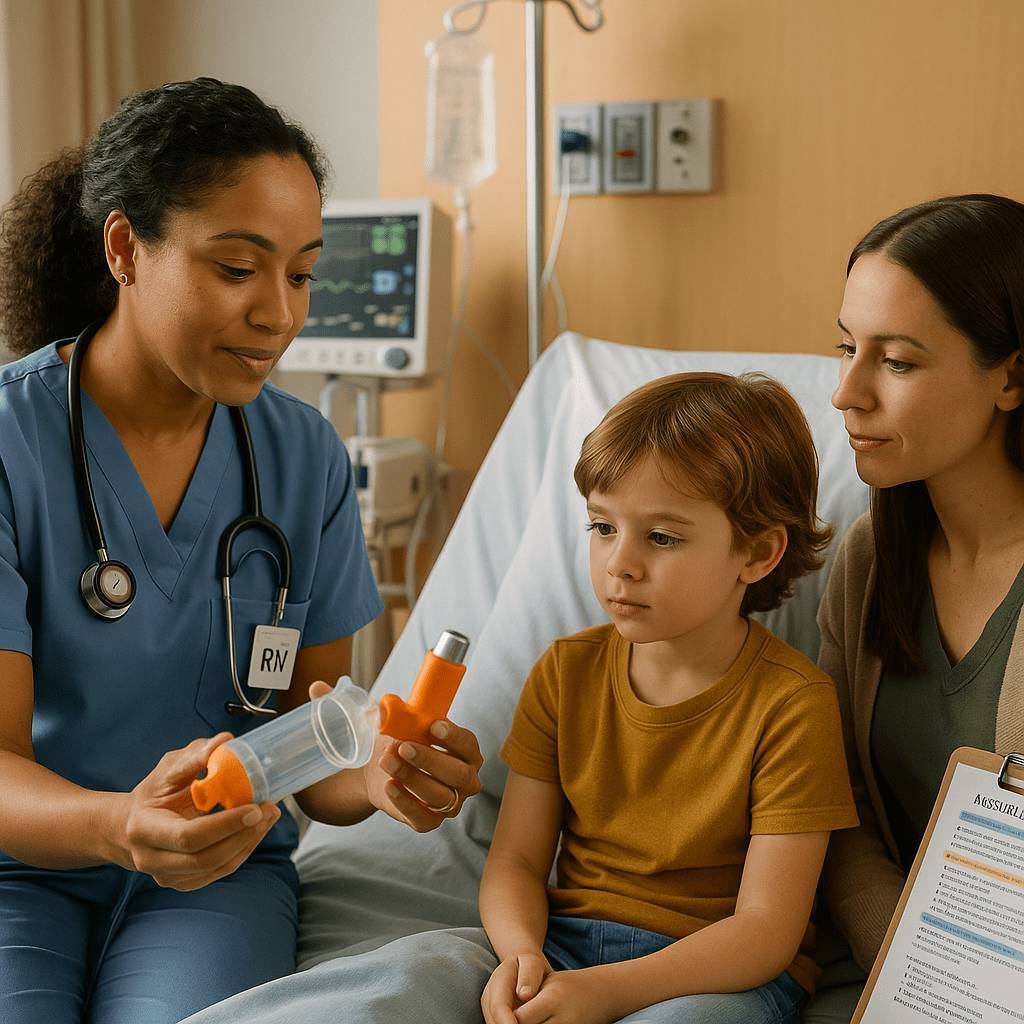
4. Spacers
Many children need a spacer for proper medication delivery. As a registered nurse, demonstrating correct use is essential.
Nursing Interventions for Asthma in Children
1. Maintain Airway and Improve Breathing
- Position child in high-Fowler’s
- Administer bronchodilators as ordered
- Provide oxygen if needed
- Monitor respiratory status closely
2. Teach the Asthma Action Plan
Every family should have a written plan describing:
- Green zone (stable)
- Yellow zone (worsening symptoms)
- Red zone (emergency)
A nurse plays a leading role in ensuring parents understand each step.
3. Trigger Avoidance Education
Help families understand how small changes can prevent hospitalizations:
- Use air purifiers
- Wash bedding frequently
- Avoid smoke exposure
- Keep pets out of sleeping areas
4. Support Emotional Needs
Children with asthma may feel scared during attacks. A calm RN nurse helps reduce anxiety, which improves breathing and cooperation.
When to Seek Emergency Care
Parents should be taught to call emergency services when:
- The child is unable to speak
- Rescue medications are not helping
- Cyanosis appears (blue lips or fingertips)
- Rapid worsening occurs
This is all heavily emphasized in NCLEX pediatric content.
Key Points for Nursing Students and Registered Nurses
- Asthma is manageable with proper education and early intervention.
- Nurses must differentiate rescue vs. maintenance medications.
- Early recognition of respiratory distress can save a child’s life.
- Patient education is one of the most important nursing roles.
❓ FAQ
Early signs include coughing, wheezing, rapid breathing, chest tightness, and use of accessory muscles. A nurse or registered nurse should assess oxygen saturation and listen for diminished breath sounds.
Short-acting beta agonists (SABA), such as albuterol, are the primary rescue medications. These drugs provide rapid bronchodilation and are essential knowledge for NCLEX preparation.
Spacers help children inhale medication slowly and more effectively. They also reduce medication loss and improve lung delivery, which is an important nursing education point.