Diabetes mellitus in children is a chronic metabolic condition that requires lifelong management and education. For every registered nurse (RN) and nursing student, understanding pediatric diabetes care is essential — both for safe clinical practice and success on the NCLEX. This guide explores the key responsibilities, interventions, and educational priorities for nurses caring for children with diabetes.
🌟 Understanding Pediatric Diabetes
Pediatric diabetes is primarily classified into Type 1 and Type 2 diabetes.
- Type 1 Diabetes occurs when the pancreas fails to produce insulin, requiring lifelong insulin therapy.
- Type 2 Diabetes involves insulin resistance and is often linked to obesity and lifestyle factors.
For nurses, recognizing early symptoms such as polyuria, polydipsia, weight loss, and fatigue is critical for timely intervention. This foundational understanding is part of every nursing bundle focused on endocrine disorders and pediatric care.
🧠 Key Nursing Responsibilities
Registered nurses play a central role in managing children with diabetes. Their responsibilities go beyond medication administration and extend into emotional support and education.
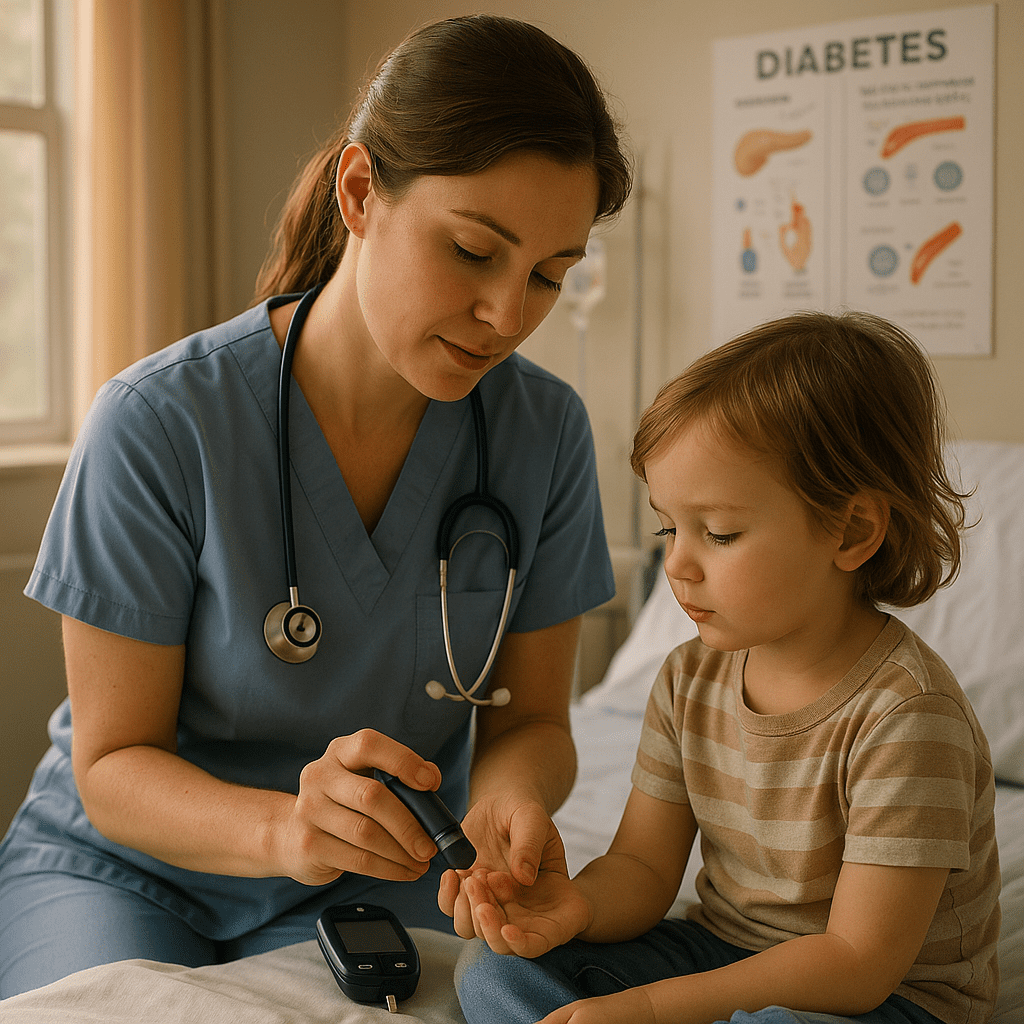
1. Monitoring Blood Glucose Levels
A nurse should ensure regular blood glucose checks before meals, at bedtime, and as needed. Proper documentation and recognizing trends help in preventing complications like hypoglycemia or hyperglycemia.
2. Administering Insulin
Insulin therapy is vital for children with Type 1 diabetes. The RN nurse must verify the correct insulin type, dose, timing, and route. Rotating injection sites and teaching families proper injection techniques are part of comprehensive nursing care.
3. Dietary Education
Teaching parents and children about balanced meals, carbohydrate counting, and snack planning is essential. The nurse collaborates with dietitians to develop individualized meal plans, which aligns with NCLEX standards for holistic care.
4. Managing Hypoglycemia and Hyperglycemia
Nurses must identify symptoms early:
- Hypoglycemia – Shakiness, sweating, irritability, confusion, seizures.
- Hyperglycemia – Excessive thirst, increased urination, fruity breath, drowsiness.
Immediate intervention and follow-up care are critical components of nursing bundles and NCLEX pharmacology scenarios.
💉 Nursing Interventions for Pediatric Diabetes
Effective diabetes management requires consistent nursing interventions focused on safety, education, and emotional support.
| Nursing Intervention | Description |
|---|---|
| Assess blood glucose trends | Identify abnormal patterns and report persistent changes. |
| Administer insulin safely | Verify dosage, timing, and monitor response. |
| Promote independence | Encourage older children to learn self-monitoring. |
| Educate families | Provide teaching on insulin storage, hypoglycemia management, and diet control. |
| Monitor for complications | Watch for signs of diabetic ketoacidosis (DKA) and infections. |
👩⚕️ Supporting Families Emotionally
Living with diabetes can be overwhelming for both the child and family. The nurse acts as an educator, counselor, and advocate — helping families cope, adhere to the care plan, and build confidence. Emotional support and reassurance are essential skills every registered nurse should master, especially when preparing for the NCLEX.
🧩 NCLEX Tips for Pediatric Diabetes Nursing
For NCLEX success, focus on:
- Recognizing signs of hypoglycemia vs. hyperglycemia.
- Prioritizing insulin safety and patient education.
- Knowing DKA management (fluids, insulin, electrolytes).
- Understanding growth and developmental needs of diabetic children.
Including these in your nursing bundle ensures readiness for clinical practice and exam performance.
🧠 Final Thoughts
Nursing care for children with diabetes requires patience, compassion, and strong educational skills. Registered nurses must empower families to take charge of diabetes management, promoting safety and independence. With proper education, consistent follow-up, and emotional support, children with diabetes can lead active, healthy lives — a goal every RN nurse strives for.
🩺 FAQs
Nurses are responsible for monitoring blood glucose, administering insulin, educating families about nutrition and self-care, and recognizing early signs of hypo- and hyperglycemia. A registered nurse (RN) also provides emotional support and coordinates with the healthcare team to ensure safe and effective diabetes management.
To prevent hypoglycemia, nurses must ensure accurate insulin administration, encourage regular meals and snacks, and educate families about carrying fast-acting glucose (like juice or glucose tablets). Consistent monitoring and documentation are key nursing interventions emphasized in NCLEX-style scenarios.
If DKA is suspected, the nurse should notify the healthcare provider immediately, start IV fluids, monitor electrolytes, and prepare to administer insulin as prescribed. Recognizing DKA symptoms—such as fruity breath, deep breathing (Kussmaul respirations), and confusion—is essential for every RN nurse working in pediatric or critical care.