Chronic autoimmune skin conditions can lead to rapid skin cell buildup, resulting in red, scaly, and itchy patches. For every registered nurse (RN), understanding these disorders is essential—not only for clinical care but also for NCLEX preparation and providing comprehensive patient education.
🧾 What You Need to Know About This Condition
These disorders occur when the immune system triggers inflammation and accelerated skin cell production. This leads to thickened, silvery plaques on the skin, often affecting the elbows, knees, scalp, and lower back. Nurses need to recognize the signs, monitor for complications, and educate patients about treatment and self-care.
⚠️ Types of Chronic Plaque Disorders
- Plaque-type Lesions (Most Common): Raised, red patches with silvery scales.
- Guttate Lesions: Small, drop-shaped patches, often triggered by infections.
- Inverse Lesions: Smooth, red areas in skin folds.
- Pustular Lesions: White pustules surrounded by red skin, rare but severe.
- Erythrodermic Presentation: Widespread redness and scaling, potentially life-threatening.
🩺 Signs and Symptoms
- Red, inflamed skin with thick plaques
- Silvery-white scales
- Itching, burning, or soreness
- Nail changes: pitting, thickening, or separation
- Flare-ups triggered by stress, infections, or medications
Nurses should carefully document these symptoms in patient charts as part of a nursing bundle to track disease progression and treatment effectiveness.
👩⚕️ Nursing Assessment and Responsibilities
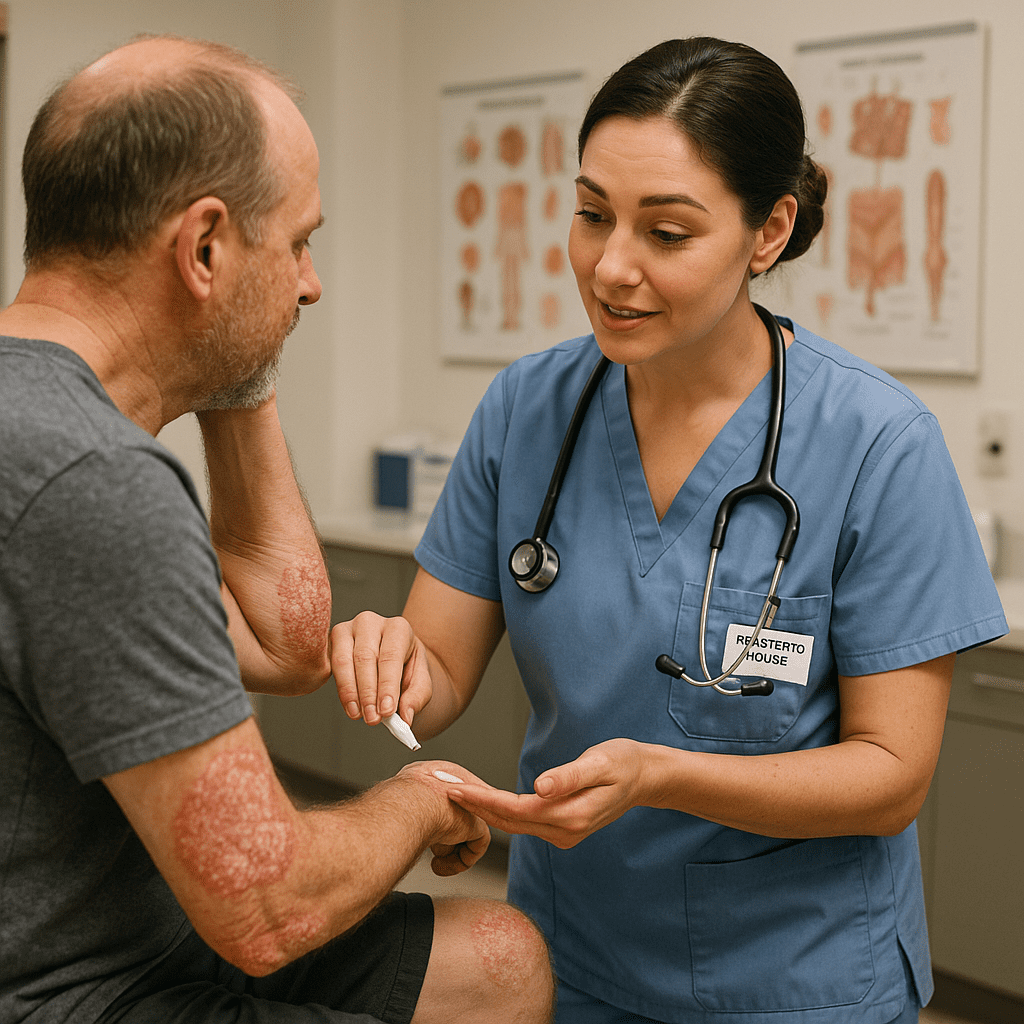
Registered nurses play a critical role in evaluating and managing chronic skin disorders:
- Skin Assessment: Monitor lesion location, size, and severity.
- Symptom Management: Provide guidance for itching relief and skin hydration.
- Patient Education: Teach about topical therapies, phototherapy, and lifestyle modifications.
- Emotional Support: Address stress, anxiety, and depression associated with chronic skin conditions.
- Medication Monitoring: Administer systemic treatments (e.g., biologics) and observe for side effects.
💊 Common Treatments Nurses Should Know
- Topical Therapies: Corticosteroids, vitamin D analogs, moisturizers
- Phototherapy: Controlled UV light exposure for severe cases
- Systemic Medications: Methotrexate, cyclosporine, or biologics (etanercept, adalimumab)
- Lifestyle Measures: Stress reduction, avoiding triggers, skin care routines
Nurses must educate patients on adherence and monitor for side effects or complications, which is essential for NCLEX scenarios focusing on chronic disease management.
🧠 NCLEX Tips for Nurses
- Identify triggers such as stress, infections, or medications.
- Know the difference between plaque-type and pustular lesions.
- Prioritize skin integrity, patient education, and emotional support.
- Remember that autoimmune skin disorders are not contagious.
🩺 FAQ: Nursing Care for Psoriasis
Psoriasis is a chronic autoimmune skin disorder causing red, scaly, and itchy plaques. Nurses must understand it to provide proper patient education, symptom management, and medication monitoring, essential skills for NCLEX and clinical practice.
The common types include:
Plaque psoriasis – raised red patches with silvery scales
Guttate psoriasis – small drop-shaped lesions
Inverse psoriasis – smooth red patches in skin folds
Pustular psoriasis – pus-filled lesions
Erythrodermic psoriasis – severe widespread redness
Nursing priorities include:
Assessing skin integrity and lesion severity
Managing itching and discomfort
Educating patients on topical and systemic therapies
Providing emotional support for stress or anxiety
Monitoring side effects of medications like biologics or corticosteroids