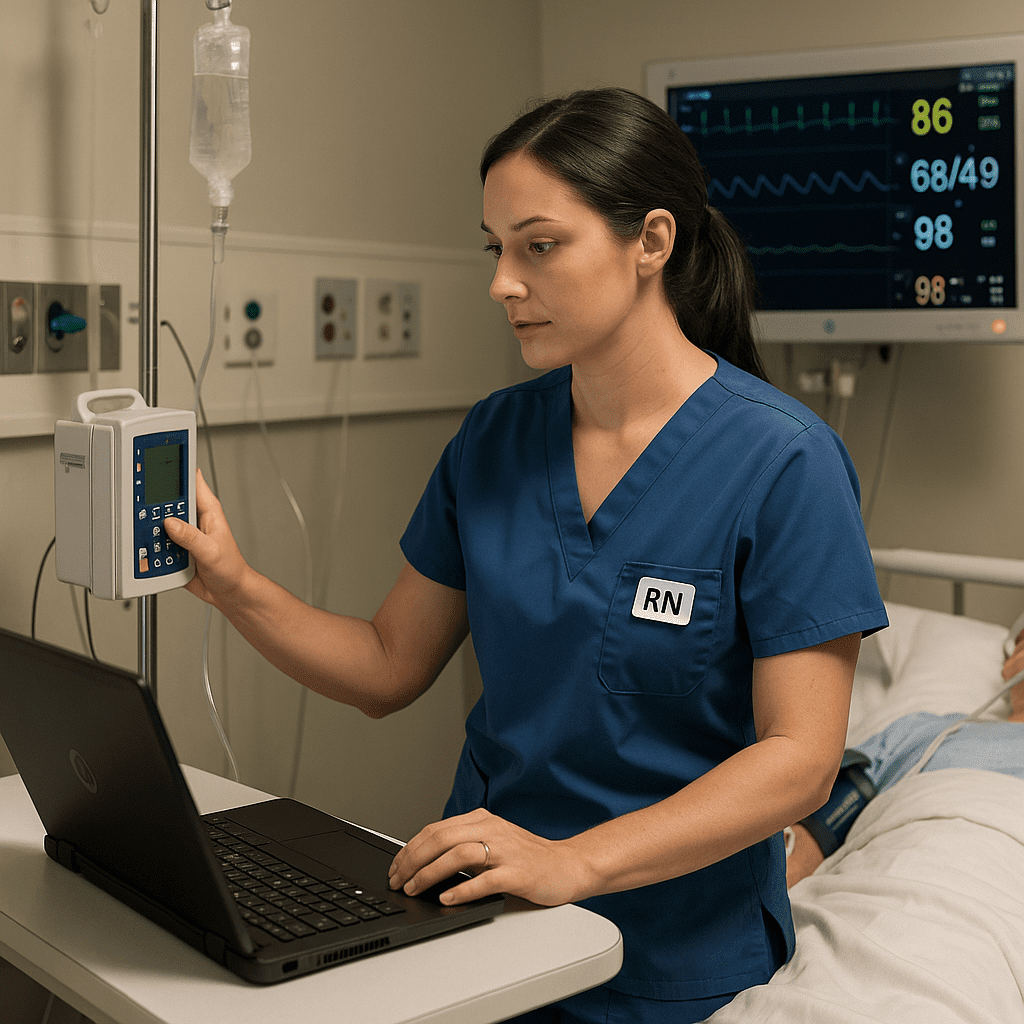
When managing patients on vasopressors, nurses play a critical role in ensuring safe administration, continuous monitoring, and early detection of complications. Vasopressors are potent medications that help restore blood pressure in patients with severe hypotension or shock. For every registered nurse (RN nurse), mastering vasopressor care is an essential skill for both clinical excellence and NCLEX success.
💉 What Are Vasopressors?
Vasopressors are medications that constrict blood vessels, increasing vascular resistance and elevating blood pressure. They’re used in life-threatening situations such as septic shock, cardiogenic shock, or severe hypotension unresponsive to fluids.
Common Vasopressors in Nursing Practice:
- Norepinephrine (Levophed)
- Epinephrine (Adrenaline)
- Dopamine
- Phenylephrine (Neo-Synephrine)
- Vasopressin
Each drug requires precise dosing, continuous monitoring, and vigilant nursing care to prevent complications like tissue necrosis or arrhythmias.
🩺 Nursing Responsibilities for Patients on Vasopressors
1. Continuous Hemodynamic Monitoring
Registered nurses must closely monitor blood pressure, heart rate, and urine output. Vasopressors can cause rapid fluctuations, so consistent monitoring is key. Use arterial lines for accurate blood pressure readings and urine output to assess perfusion.
2. Assess IV Site Frequently
Vasopressors must be administered via a central line whenever possible. If given through a peripheral line, monitor the site every 5–15 minutes for signs of infiltration or extravasation, which can lead to severe tissue damage.
3. Titrate Dosages Carefully
Vasopressors are often titrated to maintain a target mean arterial pressure (MAP)—typically ≥65 mmHg. Nurses should adjust the rate as prescribed, documenting all changes meticulously.
4. Monitor for Adverse Effects
Watch for:
- Hypertension or tachycardia
- Arrhythmias
- Peripheral ischemia (cold, pale extremities)
- Decreased urine output
Early recognition and intervention prevent serious complications.
5. Ensure Adequate Fluid Resuscitation
Before initiating vasopressors, ensure that the patient has received sufficient fluids. Starting vasopressors on a hypovolemic patient can worsen perfusion. This concept is frequently tested on the NCLEX under critical care and shock management.
⚡ NCLEX Tips for Vasopressor Management
- Always use an infusion pump for accuracy.
- Monitor MAP closely—aim for ≥65 mmHg.
- Never stop vasopressors abruptly; taper gradually as ordered.
- Assess for signs of improved perfusion (warm skin, stable vitals, adequate urine output).
- If extravasation occurs, administer phentolamine to prevent tissue necrosis.
These safety points are emphasized in NCLEX test plans and included in many nursing bundles focused on critical care.
💊 Patient Education and Collaboration
Even though patients on vasopressors are often in critical condition, nurses should communicate clearly with them and their families when possible. Explain the purpose of the medication, expected effects, and the need for close monitoring. Collaboration with physicians and pharmacists ensures safe and effective care.
🧠 Key Takeaway for Registered Nurses
Caring for patients on vasopressors requires attention to detail, strong critical thinking skills, and constant vigilance. For every RN nurse, understanding the mechanisms, side effects, and monitoring parameters of vasopressors is essential to providing safe, evidence-based care.
By mastering these responsibilities, nurses not only improve patient outcomes but also strengthen their readiness for the NCLEX and real-world clinical excellence.
FAQ: Managing Patients on Vasopressors
Vasopressors are medications that constrict blood vessels and increase blood pressure. Nurses and registered nurses (RNs) use them in critical care settings to stabilize patients with shock or severe hypotension. Understanding these drugs is essential for NCLEX preparation and nursing practice.
A nurse should closely monitor blood pressure, heart rate, urine output, and peripheral perfusion. Continuous cardiac monitoring and frequent assessment of IV site integrity are crucial to detect early signs of complications such as extravasation.
Vasopressors can cause severe tissue damage if they leak into surrounding tissues. Therefore, registered nurses prefer using a central venous line to safely administer these medications, especially in long-term or high-dose therapy.
Extravasation can cause tissue necrosis or ischemia. The nurse should immediately stop the infusion, notify the healthcare provider, and follow the hospital protocol—which often includes administering phentolamine around the affected site to reverse the vasoconstriction.