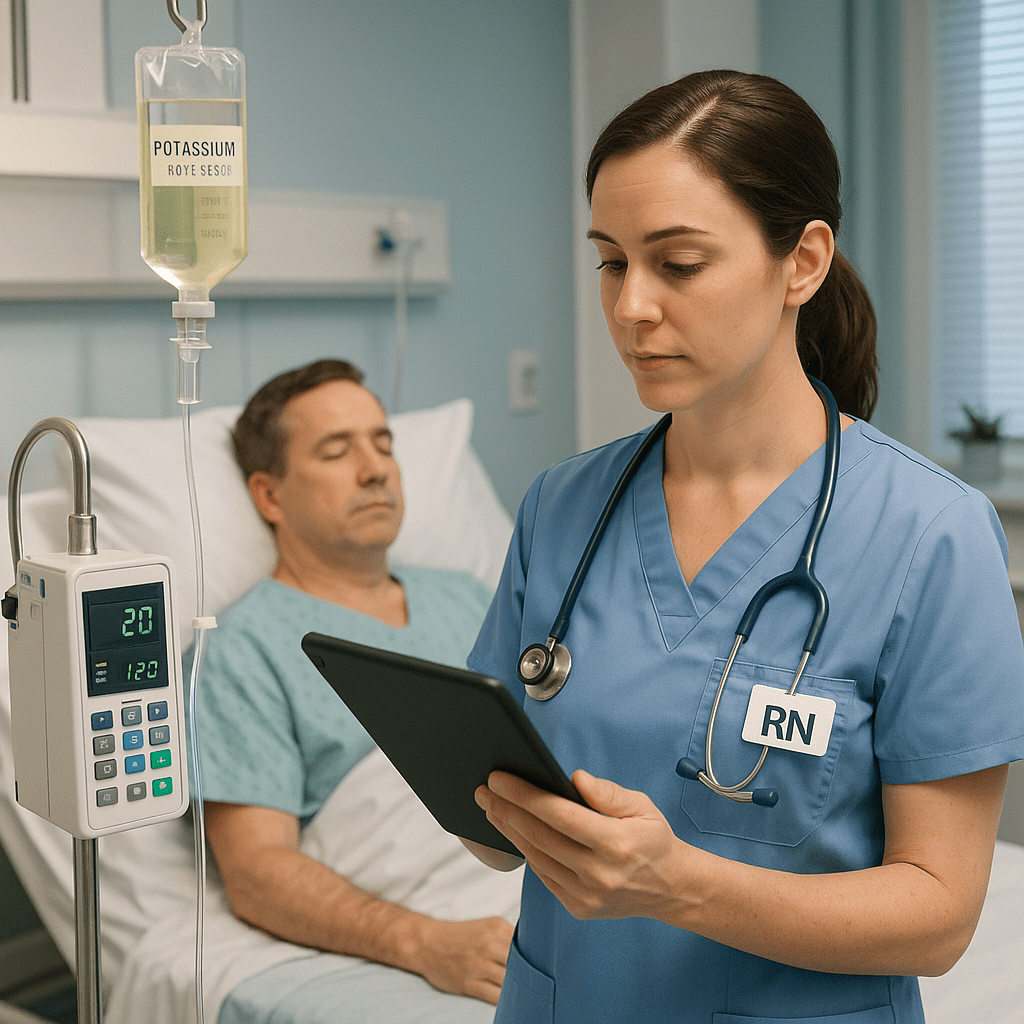
Maintaining proper electrolyte balance is a cornerstone of safe and effective nursing care. For every nurse—especially those preparing for the NCLEX—understanding electrolyte repletion protocols is critical in preventing life-threatening complications. Whether you’re a registered nurse (RN nurse) in a hospital setting or a student reviewing your nursing bundle, these protocols form the foundation for evidence-based patient management.
⚡ Why Electrolyte Repletion Matters in Nursing
Electrolytes such as potassium, sodium, magnesium, calcium, and phosphate regulate vital body functions, including cardiac rhythm, muscle contraction, and nerve signaling. When levels fall outside the normal range, the nurse must act promptly using facility-approved electrolyte replacement guidelines.
For NCLEX preparation, it’s essential to know both the signs of electrolyte imbalances and the safe nursing interventions for repletion.
🧠 Key Electrolytes and Repletion Guidelines
🩺 1. Potassium (K⁺)
- Normal Range: 3.5–5.0 mEq/L
- Replacement:
- Oral route preferred if the patient can tolerate it.
- IV potassium should never be given as a push or bolus.
- Dilute in 0.9% NaCl and infuse slowly (10–20 mEq/hr maximum).
- Nursing Care:
- Continuous ECG monitoring for cardiac rhythm changes.
- Assess renal function before administration.
- Monitor for signs of hyperkalemia (peaked T waves, muscle weakness).
💧 2. Sodium (Na⁺)
- Normal Range: 135–145 mEq/L
- Replacement:
- Hyponatremia: Administer 0.9% NaCl or hypertonic saline cautiously.
- Hypernatremia: Encourage oral fluids or administer hypotonic solutions.
- Nursing Care:
- Monitor neurological status (confusion, seizures).
- Record I&O and daily weights.
⚙️ 3. Magnesium (Mg²⁺)
- Normal Range: 1.5–2.5 mEq/L
- Replacement:
- Magnesium sulfate IV or oral supplements depending on severity.
- Avoid rapid infusion — it can cause cardiac arrest.
- Nursing Care:
- Check deep tendon reflexes (DTRs).
- Monitor respiratory status and urine output.
🦴 4. Calcium (Ca²⁺)
- Normal Range: 8.5–10.5 mg/dL
- Replacement:
- IV calcium gluconate or calcium chloride for acute cases.
- Oral calcium with vitamin D for chronic management.
- Nursing Care:
- Monitor for arrhythmias and hypotension.
- Educate patients about foods high in calcium (dairy, leafy greens).
🔬 5. Phosphate (PO₄³⁻)
- Normal Range: 2.5–4.5 mg/dL
- Replacement:
- IV phosphate (sodium or potassium phosphate) for severe deficiency.
- Oral phosphate for mild cases.
- Nursing Care:
- Monitor calcium-phosphate balance.
- Observe for tetany or muscle weakness.
🧩 Nursing Responsibilities in Electrolyte Repletion
Every registered nurse should follow these steps when implementing electrolyte replacement therapy:
- Verify lab results and assess for symptoms before replacement.
- Confirm provider orders and recheck compatibility of IV solutions.
- Use an infusion pump for accurate dosing.
- Document type, route, dose, and patient response.
- Educate the patient about diet, fluid intake, and medication interactions.
For NCLEX questions, focus on safety principles such as slow IV administration, continuous monitoring, and correct labeling of solutions.
💡 NCLEX Study Tip for Nurses
When reviewing your nursing bundle, remember these electrolyte patterns:
- Hypokalemia → Flat T waves
- Hyperkalemia → Peaked T waves
- Hypocalcemia → Positive Chvostek and Trousseau signs
- Hypermagnesemia → Depressed DTRs and bradycardia
Recognizing these cues ensures accurate prioritization and safe interventions during the NCLEX exam or clinical practice.
🩷 Final Thoughts for RN Nurses
Electrolyte repletion protocols are not just about memorizing lab values—they’re about applying critical thinking and maintaining patient safety. Every RN nurse must assess, monitor, and evaluate continuously during replacement therapy.
By mastering these nursing guidelines, you’ll strengthen your clinical judgment, improve patient outcomes, and move closer to NCLEX success.
🩺 FAQs: Electrolyte Repletion Protocols — Nursing Guidelines
Electrolyte repletion protocols are standardized nursing and medical guidelines for safely restoring abnormal electrolyte levels in patients. These protocols specify when and how to administer electrolytes like potassium, sodium, magnesium, calcium, and phosphate. They help ensure consistent, evidence-based care while minimizing the risk of complications such as arrhythmias or cardiac arrest.
Electrolyte balance is essential for maintaining cardiac rhythm, neuromuscular function, and fluid balance. For every registered nurse (RN nurse), understanding repletion protocols is vital to recognize early signs of electrolyte imbalances and provide prompt, safe interventions—key skills tested on the NCLEX exam.
The five most common electrolytes requiring repletion are potassium (K⁺), sodium (Na⁺), magnesium (Mg²⁺), calcium (Ca²⁺), and phosphate (PO₄³⁻). Deficiencies or excesses in these can cause severe cardiac, muscular, or neurological symptoms, requiring immediate nursing action.
Never administer potassium IV push — always dilute and infuse slowly.
Use an infusion pump for precise control.
Monitor the patient’s ECG and vital signs continuously.
Verify lab values and renal function before starting therapy.
Document the infusion rate, dose, and patient response carefully.