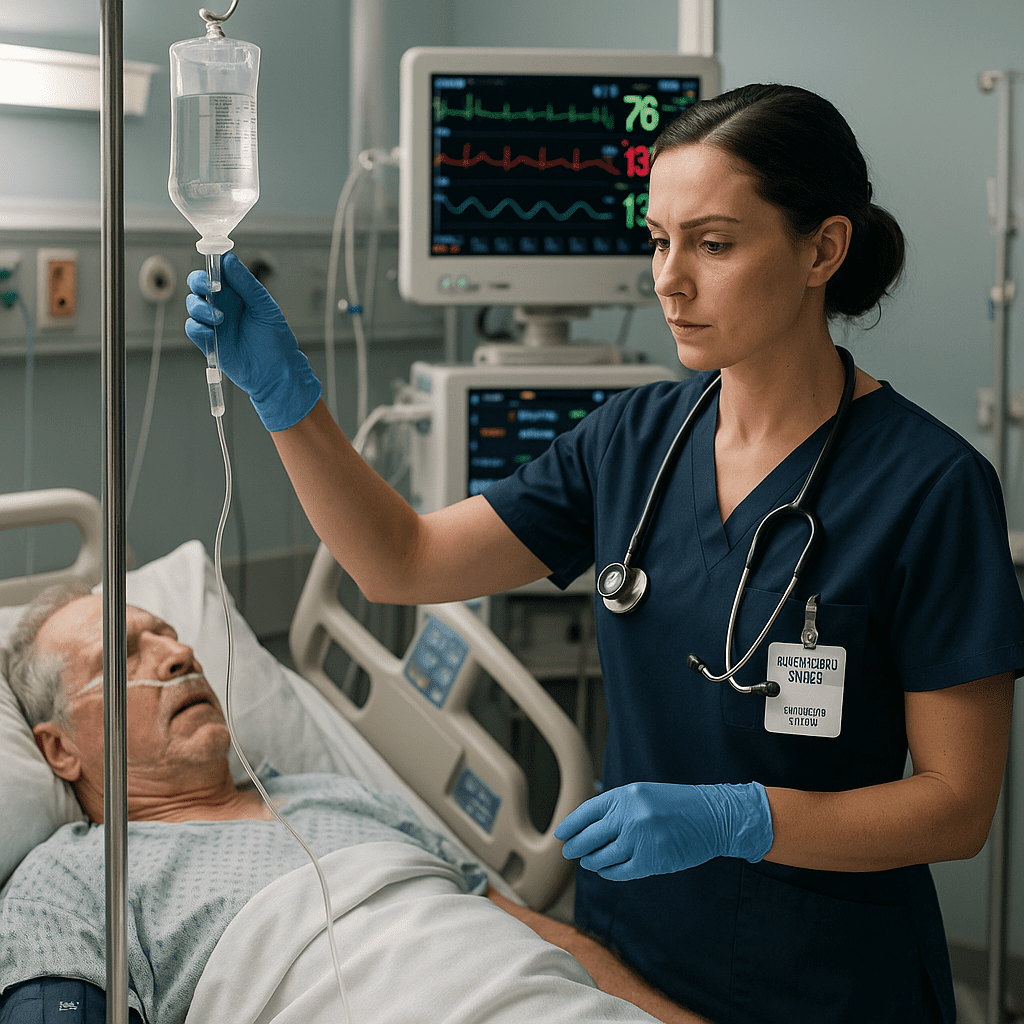
Septic shock is one of the most critical conditions that every RN nurse must recognize early. For both NCLEX preparation and real-life nursing practice, understanding the signs, symptoms, and nursing interventions for sepsis can save lives. This guide breaks down septic shock in a simple way — perfect for your nursing bundle study materials.
🧠 What Is Septic Shock?
Septic shock is a life-threatening complication of sepsis, where infection leads to dangerously low blood pressure and poor tissue perfusion. Despite fluid resuscitation, the body’s circulation fails, causing organ dysfunction.
Early detection and intervention are essential — and that’s where the registered nurse (RN) plays a key role.
⚠️ Pathophysiology Simplified
- Infection enters the bloodstream.
- The immune system releases inflammatory mediators.
- Widespread vasodilation occurs → blood pressure drops.
- Capillary permeability increases, leading to fluid leakage and edema.
- Organs become hypoxic, resulting in multi-organ failure if untreated.
🩺 Early Signs Every Nurse Must Recognize
Recognizing early sepsis symptoms before shock develops is a crucial nursing skill for both clinical and NCLEX success.
| Early (Compensated) | Late (Decompensated) |
|---|---|
| Fever or hypothermia | Hypotension despite fluids |
| Tachycardia | Cold, clammy skin |
| Rapid breathing | Altered mental status |
| Warm, flushed skin | Oliguria or anuria |
| Anxiety or restlessness | Multi-organ failure |
🔹 Tip for NCLEX nurses: “A warm patient isn’t always a stable patient.” Early septic shock may present with warm, flushed skin before perfusion fails.
💉 Nursing Assessment and Priorities
1. Vital signs & perfusion checks
- Monitor BP, HR, RR, and O₂ saturation closely.
- Watch for MAP < 65 mmHg — this indicates poor perfusion.
2. Laboratory monitoring
- Lactate > 2 mmol/L → tissue hypoxia.
- WBC count changes, elevated procalcitonin, and positive blood cultures are diagnostic clues.
3. Urine output
- < 30 mL/hr is a red flag for poor renal perfusion.
🩸 Nursing Interventions: Step-by-Step
- Call the rapid response/code team early if sepsis is suspected.
- Administer fluids (30 mL/kg crystalloid) as ordered to restore volume.
- Start broad-spectrum antibiotics ASAP — each hour of delay increases mortality.
- Monitor oxygenation and apply supplemental O₂.
- Prepare vasopressors (norepinephrine is first-line) if hypotension persists.
- Reassess continuously — vitals, urine output, mental status, and lactate levels.
- Communicate with the healthcare team about patient response.
👩⚕️ The Nurse’s Role in Preventing Septic Shock
- Recognize early sepsis triggers — infections, wounds, pneumonia, UTIs.
- Follow aseptic technique during all procedures.
- Educate patients and families on infection prevention and warning signs.
- Evaluate response to antibiotics and fluids regularly.
💡 NCLEX nursing tip: Always assess before you medicate — identifying trends in vitals or labs helps catch sepsis before it progresses to shock.
🧩 For NCLEX & Nursing Bundle Review
In your nursing bundle, remember this quick mnemonic for SEPSIS priorities:
S – Start antibiotics early
E – Evaluate lactate and labs
P – Provide fluids
S – Support oxygenation
I – Identify infection source
S – Start vasopressors if needed
🩺 Final Thoughts for the RN Nurse
Every registered nurse plays a vital role in early sepsis detection. Recognizing septic shock before it becomes irreversible is one of the most valuable skills for bedside nursing and NCLEX success. Early action saves lives — be the nurse who catches it first.
FAQs About Septic Shock in Nursing
Septic shock is a severe complication of sepsis where the body’s response to infection causes dangerously low blood pressure and tissue damage. For a registered nurse (RN nurse), early detection is crucial to prevent multi-organ failure and death.
A nurse should look for signs like fever, chills, low blood pressure (hypotension), rapid heart rate (tachycardia), confusion, and decreased urine output. Monitoring vital signs and lab results (like elevated lactate) helps nurses catch sepsis progression before shock develops — a key NCLEX nursing priority.
Registered nurses must track:
Lactate level – indicator of tissue hypoxia.
WBC count – signs of infection or immune response.
Blood cultures – to identify the causative organism.
Kidney and liver function tests – assess organ perfusion.
These are commonly tested on NCLEX and essential for nursing documentation.
Because mortality increases every hour treatment is delayed. A nurse’s rapid recognition of sepsis symptoms and prompt initiation of protocols can literally save a life. That’s why septic shock management is a high-yield NCLEX nursing topic.
Nursing bundles — like those available on RN-Nurse.com — simplify septic shock concepts through visual guides, checklists, and scenario-based practice questions. These help nursing students and registered nurses retain key interventions for the NCLEX and real-world practice.