When a Code Blue is called, seconds can mean the difference between life and death. For every nurse, especially those preparing for the NCLEX or working as a registered nurse (RN nurse), the ability to quickly read and respond to an EKG rhythm is critical. Whether you’re in the ICU, ER, or on a med-surg floor, understanding EKGs in real-time is one of the most vital skills in emergency nursing.
What Happens in a Code Blue?
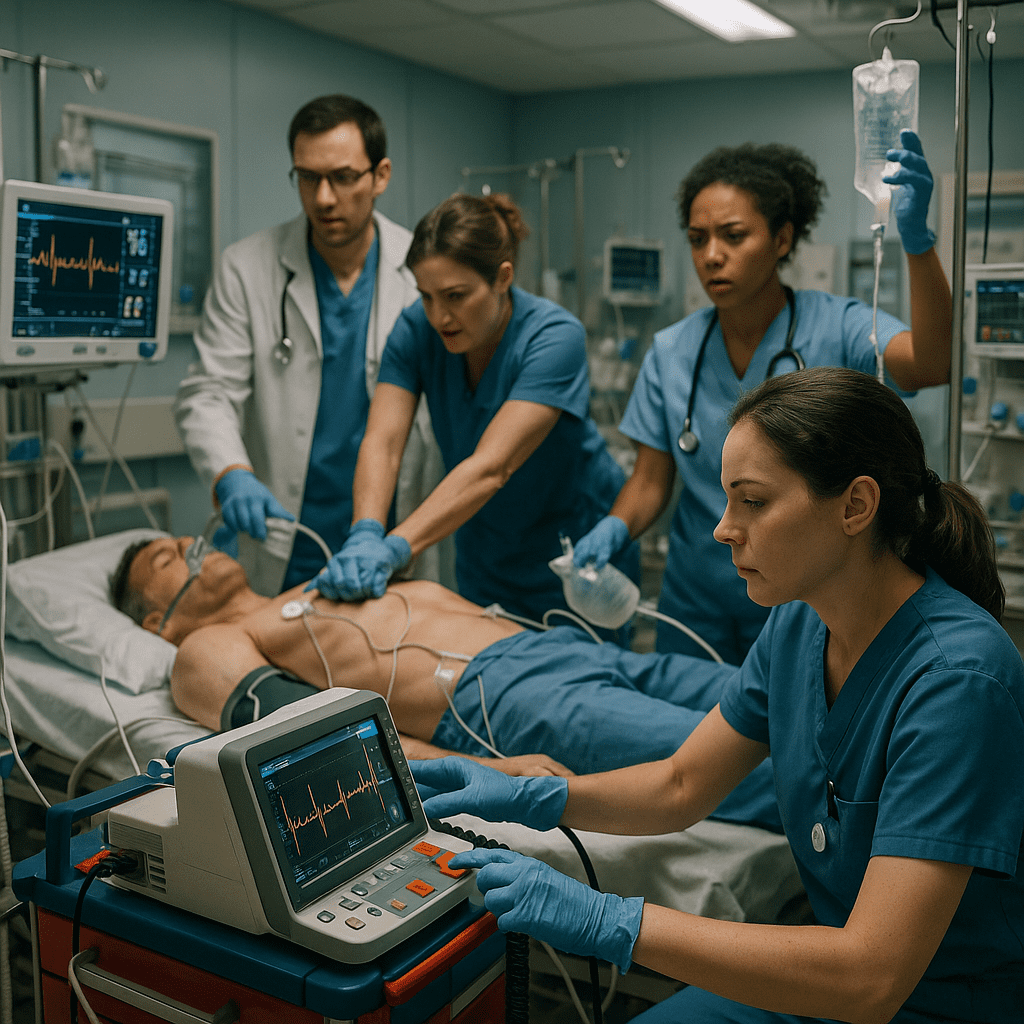
A Code Blue typically signals cardiac arrest or severe respiratory failure. During these emergencies, the team rushes to the bedside with the crash cart, oxygen, and defibrillator. The nurse is often the first responder, starting chest compressions while preparing for advanced interventions. At the same time, rapid EKG interpretation helps guide treatment decisions.
Step 1: Recognizing Shockable vs Non-Shockable Rhythms
The first priority for every registered nurse in a Code Blue is to identify whether the rhythm is:
- Shockable rhythms: Ventricular fibrillation (V-Fib) and pulseless ventricular tachycardia (V-Tach).
- Non-shockable rhythms: Asystole and pulseless electrical activity (PEA).
💡 NCLEX tip: Nurses should always initiate CPR first while preparing the defibrillator for shockable rhythms.
Step 2: Common EKG Rhythms in a Code Blue
1. Ventricular Fibrillation (V-Fib)
- Chaotic, irregular waves with no clear QRS.
- No cardiac output.
- Nursing priority: Immediate defibrillation + high-quality CPR.
2. Pulseless Ventricular Tachycardia (V-Tach)
- Wide, rapid QRS complexes.
- No palpable pulse.
- Nursing priority: Shock + CPR + prepare epinephrine/amiodarone.
3. Asystole
- Flat line, no electrical activity.
- Nursing priority: CPR + epinephrine. Do not shock.
4. Pulseless Electrical Activity (PEA)
- Organized rhythm on monitor but no pulse.
- Nursing priority: CPR + epinephrine. Search for reversible causes (the Hs and Ts).
Step 3: The Nurse’s Role in a Code Blue EKG Interpretation
Every RN nurse has key responsibilities in these situations:
- Start CPR immediately – don’t wait for the crash cart.
- Apply defibrillator pads and analyze rhythm.
- Call out EKG findings clearly so the team knows next steps.
- Assist with medications like epinephrine, amiodarone, or atropine.
- Document times, interventions, and rhythms in real-time.
Step 4: Practice With NCLEX-Style EKG Questions
One of the best ways to prepare is using nursing bundles or study sheets that focus on NCLEX emergency scenarios. Practice identifying rhythms from EKG strips and linking them to the correct interventions.
Example NCLEX-style question:
A patient is found pulseless with a wide, rapid rhythm on the EKG monitor. What is the nurse’s first action?
- A. Check the patient’s blood pressure
- B. Begin CPR and prepare for defibrillation ✅
- C. Call the physician
- D. Administer oxygen by nasal cannula
Final Thoughts
In a Code Blue, a nurse’s ability to read an EKG quickly can save lives. Recognizing V-Fib, V-Tach, Asystole, and PEA, and knowing when to shock versus when to continue CPR, are fundamental skills for every registered nurse. For NCLEX prep, focus on these rhythms, their interventions, and practice with real case-based scenarios.
Being confident in crash scenarios not only boosts your exam readiness but also makes you a stronger bedside nurse when your patients need you the most.
❓ FAQs About Reading an EKG in a Code Blue
A Code Blue is a hospital emergency that signals a patient is in cardiac or respiratory arrest. Nurses and the Code team immediately respond with CPR, EKG monitoring, and life-saving interventions.
During a Code Blue, the EKG tells the team whether the patient has a shockable rhythm (like V-fib or V-tach) or a non-shockable rhythm (like asystole or PEA). This guides whether to defibrillate, give medications, or continue CPR.
Ventricular fibrillation (V-fib) and pulseless ventricular tachycardia (V-tach) are shockable rhythms. Defibrillation is the priority intervention in these cases.
Asystole and pulseless electrical activity (PEA) are non-shockable rhythms. Treatment includes high-quality CPR, epinephrine, and searching for reversible causes (the H’s and T’s).
Registered nurses (RN nurses) monitor the patient, recognize EKG changes, deliver chest compressions or medications, prepare the defibrillator, and communicate findings to the team.
The NCLEX frequently tests Code Blue scenarios, asking nurses to identify rhythms, prioritize interventions, and apply ACLS protocols. Knowing how to read EKGs quickly is essential for passing the exam and safe practice.