Atrial fibrillation (AFib) is one of the most common cardiac arrhythmias, and it’s a critical concept for every nurse and registered nurse (RN nurse) to understand—especially when preparing for the NCLEX. As AFib directly affects cardiac output and increases the risk of life-threatening complications, nursing students must master its assessment, medications, and interventions. This guide breaks it down in a simplified way to support both clinical practice and exam readiness.
What is Atrial Fibrillation?
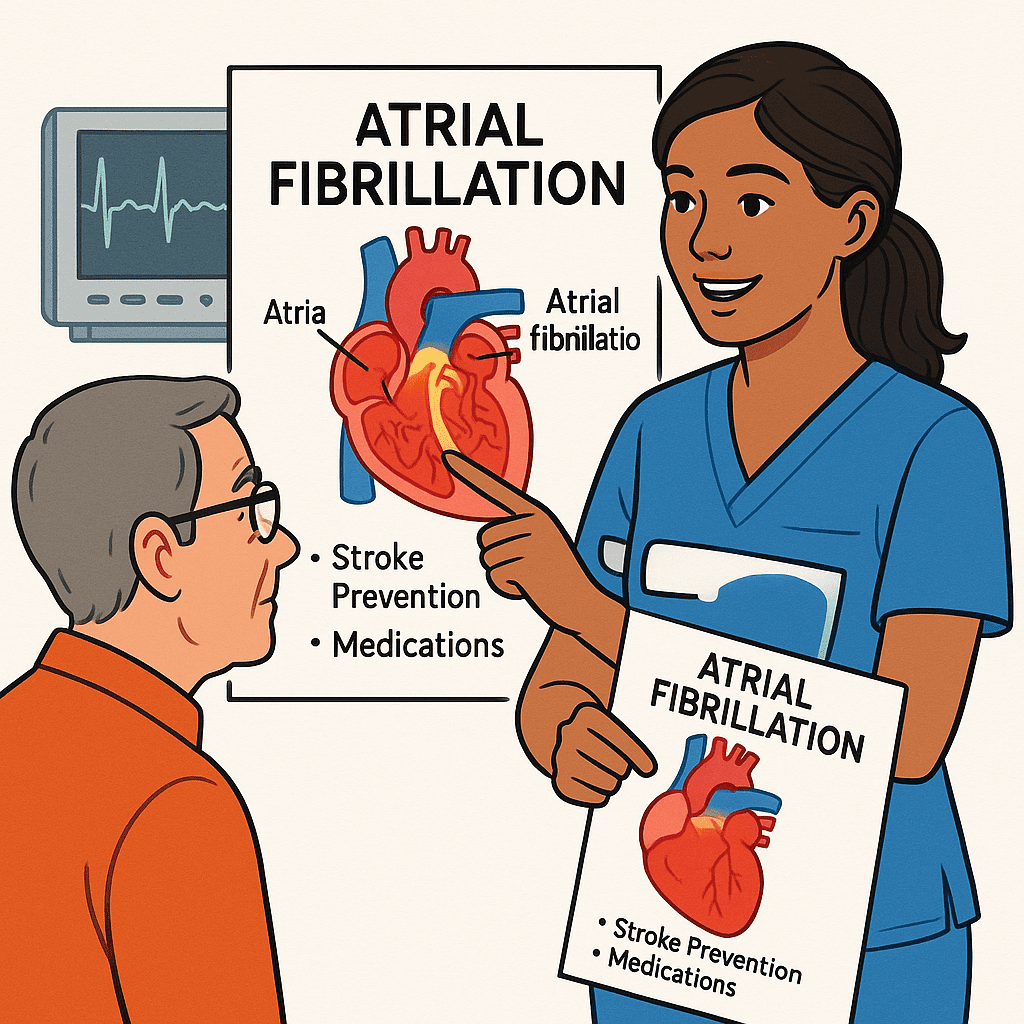
Atrial fibrillation is an irregular, often rapid heart rhythm that originates in the atria. Instead of contracting effectively, the atria “quiver,” which disrupts blood flow and increases the risk of clot formation.
- ECG finding: No distinct P waves, irregular R-R intervals, and a fibrillatory baseline.
- Key nursing bundle point: The absence of P waves is one of the most tested NCLEX clues.
Risks Associated with Atrial Fibrillation
Every nurse should remember that AFib isn’t just about an irregular rhythm—it’s about what it can cause:
- Stroke risk (most critical): Stagnant blood can lead to clot formation in the atria, which may travel to the brain.
- Heart failure: Due to decreased cardiac output and poor ventricular filling.
- Decreased perfusion: Fatigue, dizziness, hypotension, and syncope.
- Compromised quality of life: Anxiety, palpitations, and activity intolerance.
💡 NCLEX tip: If an NCLEX question asks about the most life-threatening risk of atrial fibrillation, the answer is stroke.
Medications for Atrial Fibrillation
Nurses must be able to identify the main classes of medications used for AFib management.
- Anticoagulants – Prevent stroke
- Examples: Warfarin, Apixaban, Rivaroxaban.
- Nursing tip: Monitor INR for patients on warfarin.
- Rate control medications – Slow the ventricular response
- Beta blockers: Metoprolol.
- Calcium channel blockers: Diltiazem, Verapamil.
- Rhythm control medications – Restore sinus rhythm
- Amiodarone, Sotalol.
- Digoxin – Sometimes used for rate control, especially in older patients.
Nursing Interventions for Atrial Fibrillation
A registered nurse plays a crucial role in AFib management. Nursing care includes:
- Monitor vital signs and ECG: Watch for worsening arrhythmias or rapid ventricular response.
- Educate about anticoagulation: Teach patients about bleeding risks, INR checks, and medication adherence.
- Assess for complications: Watch for stroke signs (sudden weakness, slurred speech).
- Prepare for procedures: Cardioversion, ablation, or pacemaker insertion may be ordered.
- Promote lifestyle changes: Low-sodium diet, exercise, stress management, and avoiding stimulants (like caffeine).
Atrial Fibrillation and the NCLEX
For nursing students, AFib often appears in NCLEX-style questions. Key testable points include:
- Recognition of ECG findings.
- Prioritizing stroke risk.
- Knowing first-line medications and safety teaching.
- Understanding when cardioversion is appropriate (e.g., only if the patient has been anticoagulated to reduce clot risk).
If you are preparing for the exam, using a nursing bundle with EKG nursing sheets can make it easier to recognize rhythms quickly.
Final Thoughts
Atrial fibrillation is a high-yield topic for both clinical practice and the NCLEX. Every RN nurse must be ready to assess, intervene, and educate patients on AFib risks, medications, and safety. With proper preparation—such as reviewing a nursing bundle focused on EKG rhythms—you’ll feel confident in both exams and real-world nursing care.
❓ Atrial Fibrillation Nursing – FAQs
A: The greatest risk is stroke due to blood clot formation in the atria. Nurses and registered nurses must monitor anticoagulation therapy closely.
A: Beta-blockers, calcium channel blockers, digoxin, and anticoagulants are key. Nursing bundles often include medication charts for NCLEX prep.
A: Monitor ECG, assess for signs of stroke, educate patients about medication adherence, and prepare for possible cardioversion if ordered.
A: In simple words: “Your heart is beating irregularly, which may cause blood clots. Medicines help control the rhythm and prevent stroke.”
A: Expect scenario-based questions like “Hold or give this medication?” or identifying atrial fibrillation on an ECG strip (irregularly irregular rhythm).