Congenital heart defects (CHDs) are some of the most important topics nursing students must understand for the NCLEX and for safe patient care. These defects are structural heart problems present at birth, and they can greatly affect a child’s circulation and oxygenation. Therefore, as a registered nurse (RN) or nursing student, knowing the difference between cyanotic and acyanotic heart defects is essential for effective care.
🔹 What Are Congenital Heart Defects?
A congenital heart defect occurs when the heart or its major vessels do not form properly during fetal development. In fact, these defects vary in severity—ranging from minor issues that may resolve on their own to life-threatening conditions that require surgical intervention.
For the NCLEX, you’ll frequently encounter questions about:
- Types of CHDs
- Cyanotic vs. Acyanotic differences
- Nursing care and monitoring
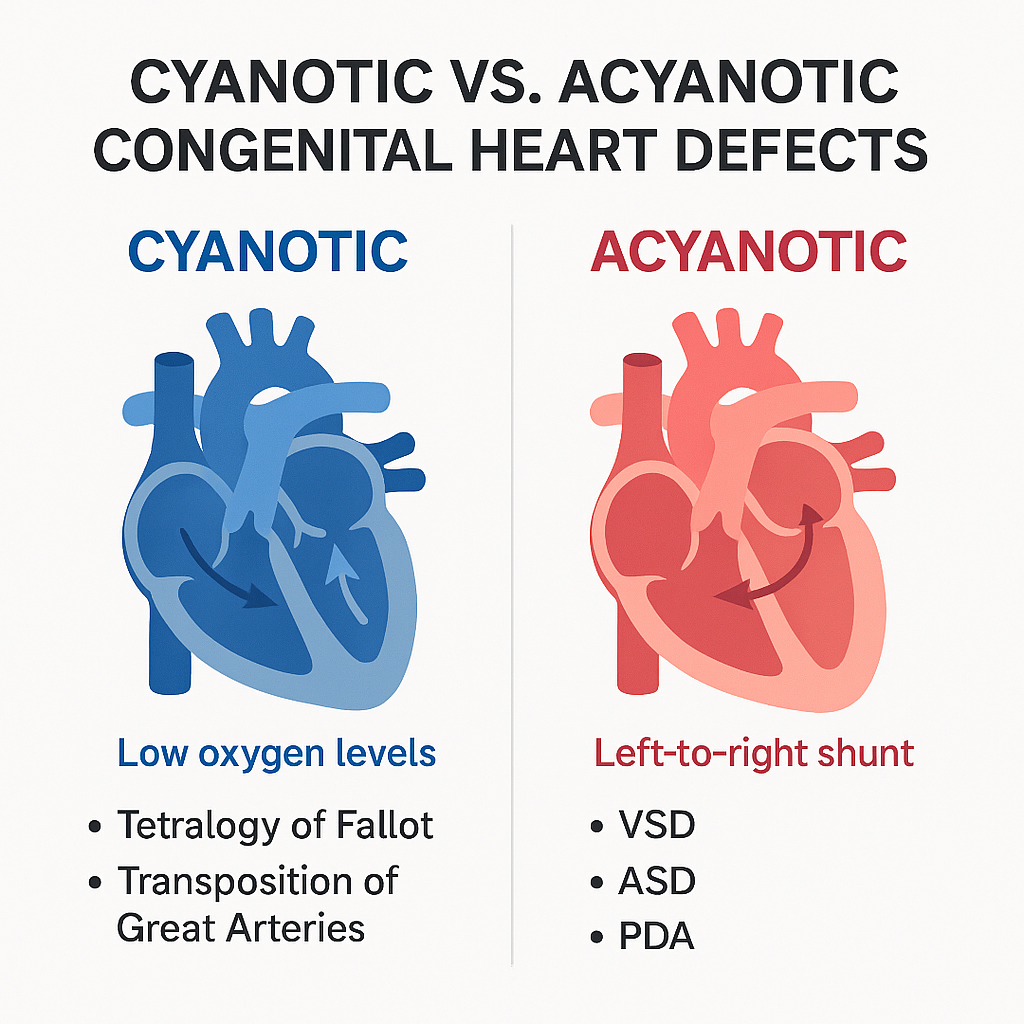
🔹 Cyanotic vs. Acyanotic Heart Defects
✅ Cyanotic Defects
Definition: Cyanotic heart defects cause low oxygen levels in the blood, leading to blue-tinged skin (cyanosis).
Key Examples:
- Tetralogy of Fallot (TOF)
- Transposition of the Great Arteries (TGA)
Pathophysiology: In these cases, blood either bypasses the lungs or mixes oxygen-poor and oxygen-rich blood. As a result, oxygen delivery to the tissues is reduced.
Signs & Symptoms:
- Cyanosis (blue lips, nails)
- Clubbing of fingers
- Difficulty feeding
- Fatigue during activity
✅ Acyanotic Defects
Definition: Acyanotic defects do not cause cyanosis because oxygenation is usually adequate. However, the extra blood flow may place additional strain on the heart.
Key Examples:
- Atrial Septal Defect (ASD)
- Ventricular Septal Defect (VSD)
- Patent Ductus Arteriosus (PDA)
Pathophysiology: These defects usually involve a left-to-right shunt, which causes increased blood flow to the lungs.
Signs & Symptoms:
- Heart murmur
- Frequent respiratory infections
- Poor weight gain
🔹 Nursing Priorities for Cyanotic and Acyanotic CHDs
As a nurse or RN, your role includes early recognition, monitoring oxygen levels, and educating families. Moreover, these priorities are frequently tested on the NCLEX.
For Cyanotic Defects
- Administer oxygen as ordered, but keep in mind that oxygen may not fully correct cyanosis.
- Prepare for surgical interventions or cardiac catheterization.
- Monitor for Tet Spells (acute cyanosis during crying or feeding); in such cases, place the infant in the knee-chest position to increase systemic vascular resistance.
For Acyanotic Defects
- Monitor for signs of congestive heart failure (tachypnea, edema).
- Administer medications such as diuretics or digoxin as prescribed.
- In addition, teach parents about feeding techniques to prevent fatigue.
🔹 NCLEX Tips for CHDs
- Mnemonic:
- Cyanotic = C for “color change (blue)” and includes right-to-left shunts.
- Acyanotic = A for “adequate oxygenation” but left-to-right shunts.
- Common NCLEX questions focus on:
- Pathophysiology differences
- Signs and symptoms
- Priority interventions
🔹 Why Nurses Need to Master CHDs
Understanding CHDs is critical for nursing care in pediatric and neonatal units. Consequently, whether you are a registered nurse (RN) preparing for the NCLEX or a student using a nursing bundle for study, mastering these differences ensures safe patient care and exam success.
🔹 Final Thoughts
Congenital heart defects are complex. However, with the right approach, they become manageable. To summarize, remember the key differences:
- Cyanotic = blue babies (low oxygen).
- Acyanotic = pink babies (adequate oxygen, but overworked heart).
As a nurse, your role is not only to monitor and educate but also to act quickly when signs of distress appear. Therefore, mastering these concepts will bring you closer to both NCLEX success and safe patient outcomes.
❓FAQs: Acyanotic Congenital heart disease
Definition of Cyanotic Defects:
A cyanotic congenital heart defect is present at birth and involves mixing of oxygen-rich and oxygen-poor blood. As a result, less oxygen reaches the body.
Definition of Acyanotic Defects:
In contrast, acyanotic defects don’t usually cause blood mixing. Instead, they may involve excess blood flow or pressure load, but oxygen saturation generally stays normal.
Key Differences in Symptoms:
Cyanotic defects often show bluish skin, lips, or nails, whereas acyanotic defects may present subtly, such as murmurs or shortness of breath on exertion.
List of Common Cyanotic Defects:
Tetralogy of Fallot
Transposition of the Great Arteries
Truncus Arteriosus
Pulmonary Atresia
Total Anomalous Pulmonary Venous Return
Hypoplastic Left Heart Syndrome
Tricuspid Valve abnormalities
Note: For instance, Tetralogy of Fallot is often diagnosed in infants due to cyanosis and low oxygen levels.
List of Common Acyanotic Defects:
Ventricular Septal Defect (VSD)
Atrial Septal Defect (ASD)
Patent Ductus Arteriosus (PDA)
Pulmonary Stenosis
Aortic Stenosis
Coarctation of the Aorta
Additional Info: Moreover, oxygenated blood usually circulates normally, so cyanosis is rarely seen.
Symptoms in Cyanotic Defects:
Cyanotic defects often show bluish discoloration, low oxygen saturation, and rapid breathing.
Symptoms in Acyanotic Defects:
Acyanotic defects may present subtly, including heart murmurs or shortness of breath during activity. Therefore, proper assessment is crucial for diagnosis.
Diagnostic Tools:
Echocardiograms
Chest X-rays
Electrocardiograms (ECG)
Pulse oximetry
Cardiac catheterization (in complex cases)
Importance: In addition, early diagnosis allows timely treatment and better outcomes.
Treatment for Acyanotic Defects:
Management may include medications, catheter procedures, or surgery if needed.
Treatment for Cyanotic Defects:
Cyanotic defects often require urgent surgery or palliative interventions. Thus, nurses must monitor patients closely and be prepared for emergency care.