Administering medications to pediatric patients is one of the most important responsibilities of every registered nurse (RN). It requires precision, a solid understanding of developmental stages, and strict adherence to safety protocols. Whether you’re preparing for the NCLEX or improving your clinical skills, mastering pediatric medication administration is essential for safe, effective nursing care.
In this guide, we’ll walk you through dosing principles, routes of administration, and key safety strategies every RN nurse should follow.
✅ Why Pediatric Medication Administration Is Different
Unlike adults, children have unique physiological characteristics that influence absorption, distribution, and metabolism of medications. Their organs are still developing; therefore, dosages must be calculated carefully based on weight (mg/kg) or body surface area (BSA). Even a small mistake can cause serious complications. Consequently, accuracy and double-checking are top priorities for every registered nurse.
Moreover, children’s responses to drugs can vary significantly, making it vital to observe for side effects and adjust doses promptly.
✅ Key Principles for Pediatric Medication Dosing
1. Weight-Based Calculations:
Most pediatric doses are based on the child’s weight. Always weigh the patient in kilograms to ensure precision.
2. Double-Check All Calculations:
Medication errors remain one of the leading causes of pediatric harm. Thus, use a second nurse to verify every critical calculation whenever possible.
3. Use the Right Formula:
![]()
4. Check the Maximum Dose:
Never exceed the adult maximum dose unless the prescriber clearly directs it.
Example:
If the order is 10 mg/kg of acetaminophen every 6 hours for a child weighing 15 kg:
10 × 15 = 150 mg per dose.
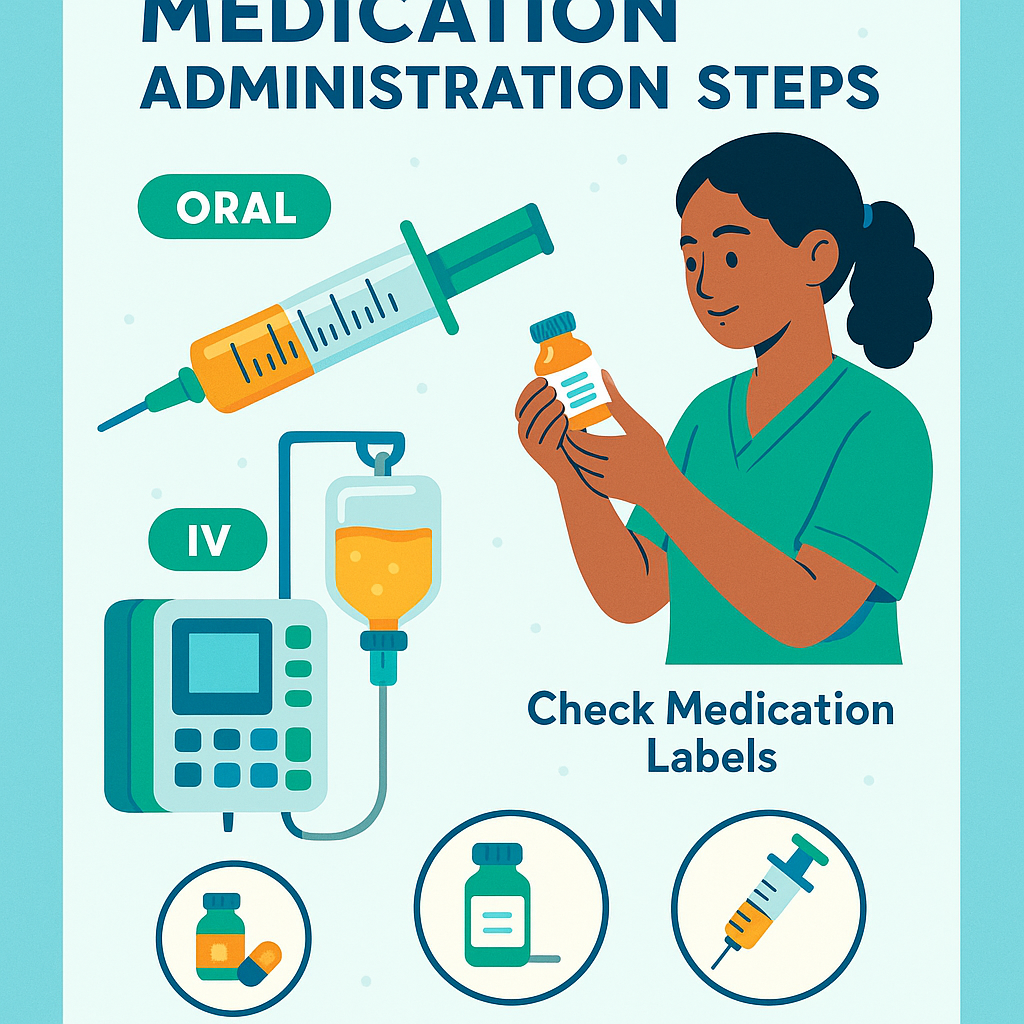
✅ Common Routes of Pediatric Medication Administration
💊 Oral Route (PO)
This is the most common route for pediatric patients. Whenever possible, use liquid formulations or crush tablets (if allowed) for easier swallowing. Additionally, always use oral syringes for accuracy and avoid household spoons.
💉 Intravenous (IV)
IV administration is used for severe illnesses or when the child cannot take oral medications. Therefore, using infusion pumps is essential to prevent fluid overload.
💪 Intramuscular (IM)
Choose the correct injection site:
- Vastus lateralis (thigh) for infants
- Deltoid for older children
Use an appropriate needle size and limit volume per injection to prevent tissue injury.
🧸 Rectal Route
This route is a good alternative for children who are vomiting or unable to take oral medications. However, always confirm medication compatibility before using this method.
✅ Safety Tips for Pediatric Medication Administration
To ensure patient safety, every RN nurse should follow these six rights of medication administration:
- Right patient
- Right drug
- Right dose
- Right route
- Right time
- Right documentation
Additionally:
- Educate parents and caregivers about dosing schedules and potential side effects using simple language.
- Use age-appropriate tools such as syringes, droppers, or calibrated cups.
- Check for allergies and drug interactions, particularly when administering antibiotics or pain medications.
- Avoid adult assumptions — children are not small adults; their physiology differs in key ways.
Furthermore, always stay calm and reassuring when medicating children, as your tone can significantly influence their cooperation.
✅ High-Risk Medications for Children
Some medications require extra caution:
- Insulin: Must be dosed precisely to avoid hypoglycemia.
- Opioids: Use sparingly, as they increase the risk of respiratory depression.
- Antibiotics: Always adjust doses based on renal and hepatic function.
Therefore, close monitoring and proper education are vital after administration.
✅ NCLEX & Nursing Practice Tips
You can expect NCLEX questions on weight-based dosing, calculation safety, and medication administration routes. For success, remember to:
- Memorize safe dosage ranges for common pediatric medications.
- Know which routes and needle sizes are appropriate for each age group.
- Apply prioritization: safety, dose verification, and documentation come first.
In addition, integrating this topic into your nursing bundle helps reinforce essential knowledge for med-surg and pediatric nursing exams.
✅ Final Thoughts
Ultimately, administering medications to children demands accuracy, patience, and strong communication skills. By combining precise calculations with evidence-based safety practices, you can ensure the highest level of pediatric care.
Furthermore, mastering these concepts not only boosts your clinical confidence but also enhances your performance on the NCLEX. For more structured learning, include pediatric pharmacology in your Nursing Bundle to strengthen both your knowledge and your patient care outcomes.