Introduction
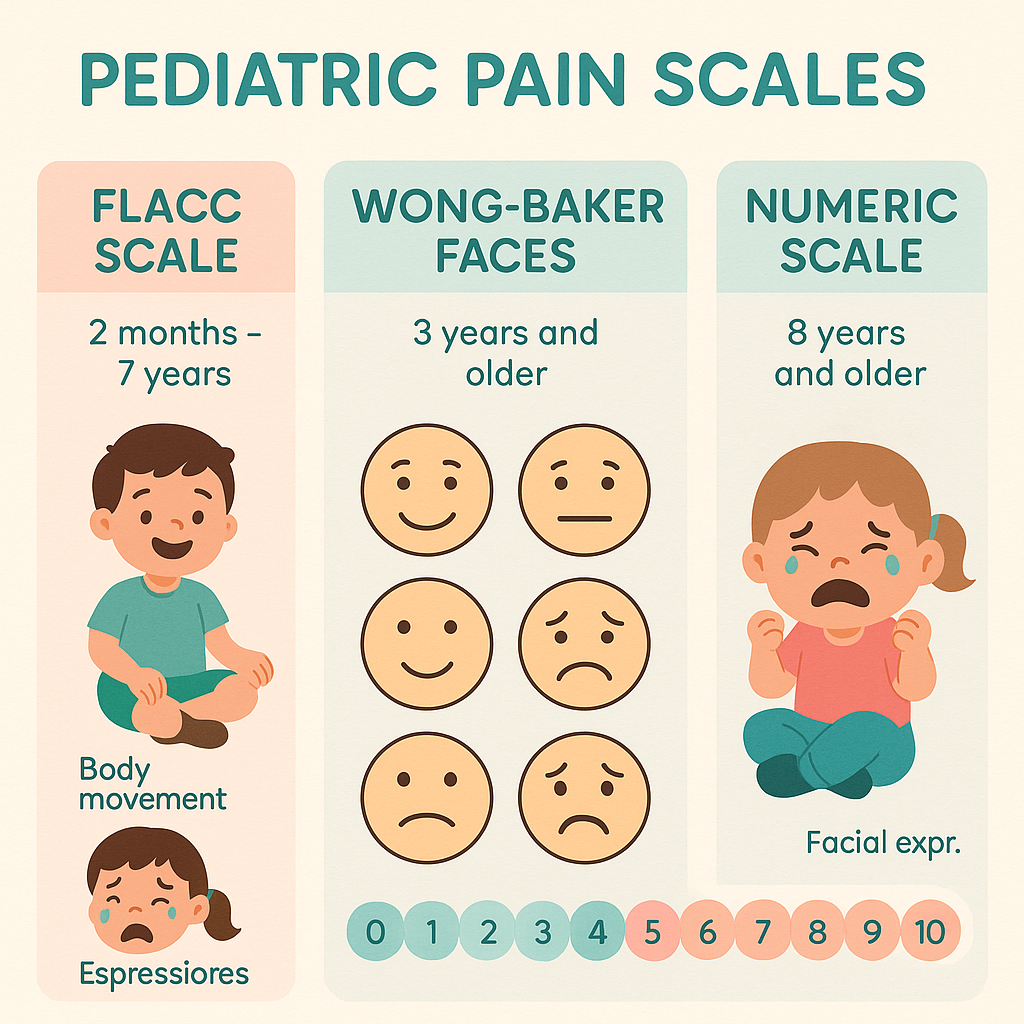
Pediatric patients can’t always describe their pain clearly. That’s why nurses must rely on pain assessment tools designed specifically for children. Whether you’re a registered nurse (RN nurse), nursing student, or prepping for the NCLEX, understanding pain scales like FLACC, Wong-Baker, and the Numeric Rating Scale is essential for accurate and compassionate care.
This guide breaks it down—simple, nurse-friendly, and clinical-ready.
Why Pain Assessment Matters in Pediatrics
In children, untreated pain can lead to complications like anxiety, delayed healing, and behavior issues. As a nurse, your ability to assess pain and document it correctly helps provide timely interventions and improves patient outcomes.
1. FLACC Scale (For Infants and Nonverbal Children)
What It Stands For:
- Face
- Legs
- Activity
- Cry
- Consolability
Who It’s For:
- Ages: 2 months to 7 years (especially nonverbal or pre-verbal children)
How It Works:
Each category is scored from 0 to 2. Total score ranges from 0 (no pain) to 10 (severe pain).
| Category | 0 | 1 | 2 |
|---|---|---|---|
| Face | No expression/smile | Occasional frown/grimace | Constant frown, clenched jaw |
| Legs | Normal movement | Uneasy, tense | Kicking, drawn-up legs |
| Activity | Quiet, normal | Squirming, tense | Rigid, jerking |
| Cry | No cry | Moans/whimpers | Constant crying, screams |
| Consolability | Content | Reassured by touching/talking | Difficult to console |
Nurse Tip: Use this scale often in pediatric med-surg units and PICUs. Know it for the NCLEX and your nursing bundle cheat sheets!
2. Wong-Baker FACES Scale
Who It’s For:
- Children 3 years and older
- Verbal children who can point to pictures
How It Works:
- Children are shown faces ranging from a happy face (0) to a crying face (10).
- The child points to the face that best matches how they feel.
Key Advantage:
- Easy to understand
- Quick visual communication tool
Nurse Tip: Always ask the child what the selected face means to them before assigning a numeric value. This builds rapport with patients and their families, which is critical in nursing care.
3. Numeric Rating Scale (NRS)
Who It’s For:
- Children 8 years and older
- Those who can understand and use numbers
How It Works:
- Ask: “On a scale from 0 to 10, how bad is your pain?”
- 0 = no pain; 10 = worst possible pain
Nurse Tip:
Combine the NRS with vital signs, physical cues, and the child’s behavior for the most accurate assessment.
Choosing the Right Scale
| Age Group | Best Pain Scale |
|---|---|
| 0–2 years | FLACC |
| 3–7 years | Wong-Baker FACES |
| 8+ years | Numeric Rating Scale |
Documenting Pediatric Pain
As a registered nurse, it’s not enough to assess pain—you must also document it accurately. Use EHR systems to record:
- Pain score
- Time of assessment
- Intervention (e.g., Tylenol, distraction)
- Response to treatment
Good documentation helps guide treatment, protects legal integrity, and supports NCLEX clinical scenarios.
Tips for NCLEX and Clinical Practice
✅ Memorize when to use each scale based on age
✅ Combine pain scale results with clinical judgment
✅ Involve parents or caregivers when possible
✅ Monitor for nonverbal signs of pain in infants or developmentally delayed children
✅ Reassess pain 30–60 minutes after intervention
Why This Matters in NCLEX and Practice
Pain questions are common on the NCLEX, especially around pediatric and mental health nursing. Mastering these tools ensures you’re prepared for exams and real-life clinical scenarios.
Whether you’re building your nursing bundle or reviewing peds care, pain scales are a must-know.
Conclusion
Pain in children can be tricky to detect—but with the right tools, nurses can confidently provide comfort, safety, and care. By mastering the FLACC, Wong-Baker, and Numeric Rating Scales, you’ll ensure better outcomes for young patients and ace your NCLEX.