Introduction
Respiratory distress in children is a critical condition that every registered nurse (RN) and nursing student should recognize and respond to fast. Children, especially infants and toddlers, can deteriorate quickly. Whether you’re studying for the NCLEX or working in a pediatric or emergency unit, understanding the signs, nursing interventions, and red flags can save lives.
What Is Respiratory Distress?
Respiratory distress means a child is working harder to breathe. It’s not just fast breathing—it’s the body showing it’s struggling to get enough oxygen. This is different from respiratory failure, which is more severe and may require emergency interventions like intubation.
Common Causes of Respiratory Distress in Kids
- Bronchiolitis
- Asthma
- Pneumonia
- Croup
- Foreign body aspiration
- Congenital abnormalities
- Allergic reactions or anaphylaxis
Nurses must assess the underlying cause to provide proper care.
Early Signs to Watch For
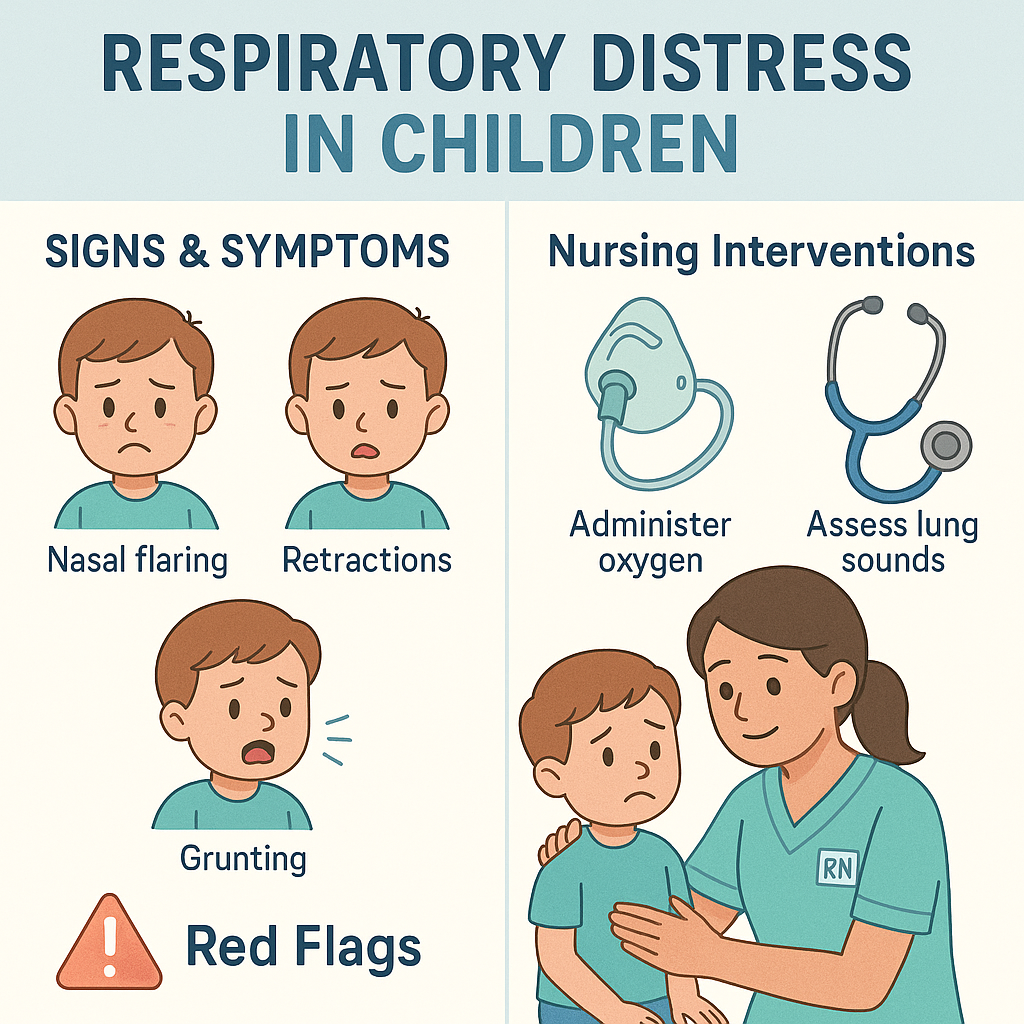
Spotting early signs gives nurses and caregivers a chance to intervene before the child crashes. Look for:
- Tachypnea (rapid breathing)
- Nasal flaring
- Retractions (using neck, chest, or abdominal muscles to breathe)
- Grunting
- Head bobbing
- Increased work of breathing
- Restlessness or irritability
👉 NCLEX tip: Grunting and nasal flaring in infants are always red flags.
Nursing Assessment: What to Monitor
Every RN nurse should use a systematic approach to assess respiratory distress. Here’s a quick guide:
| Assessment Area | What to Check |
|---|---|
| Airway | Is it open and clear? Any sounds like stridor or wheezing? |
| Breathing | Respiratory rate, rhythm, effort. Are there retractions or grunting? |
| Circulation | Skin color, capillary refill, pulse ox reading |
| Mental Status | Alert, irritable, lethargic |
| Vital Signs | Watch trends in HR, RR, BP, O2 sat |
Key Interventions for Nurses
When you recognize respiratory distress, act fast. Your nursing interventions will vary depending on the severity:
Mild to Moderate Distress
- Elevate the head of the bed
- Administer oxygen via nasal cannula or mask
- Monitor O2 saturation continuously
- Stay calm and keep the child comfortable
- Notify the healthcare provider promptly
Severe Distress or Deterioration
- Activate rapid response team or code blue
- Bag-mask ventilation if O2 sat drops too low
- Prepare for possible intubation
- Assist with medications (bronchodilators, steroids, epinephrine)
💡 NCLEX reminder: Always apply oxygen FIRST if a child shows signs of hypoxia.
Red Flags You Can’t Ignore 🚨
These are signs the child may be heading toward respiratory failure:
- O2 saturation below 90% despite oxygen
- Lethargy or unresponsiveness
- Silent chest (no air movement)
- Bradycardia (late sign)
- Apnea or gasping
- Cyanosis (especially around lips)
If you see any of these, this is an emergency. Call for help immediately and prepare to support breathing.
Communication and Documentation
Nursing documentation is critical in respiratory distress. Make sure to chart:
- Respiratory rate and effort
- O2 delivery method and response
- Reassessment findings
- Interventions taken
- Communication with the healthcare team
This is not just important for patient safety—it’s also a key NCLEX topic and a nursing bundle priority.
Nurse’s Role in Family Support
As a registered nurse, don’t forget the emotional support side. Parents are often scared. Use therapeutic communication to explain what’s happening and what you’re doing to help.
Examples:
- “We’re giving your child oxygen to help them breathe easier.”
- “It looks scary, but we are watching your child very closely and acting fast.”
NCLEX Style Review Question
Question:
A nurse is assessing an infant who is grunting, has nasal flaring, and is retracting. What is the nurse’s FIRST action?
A. Call respiratory therapy
B. Start chest compressions
C. Apply oxygen and monitor O2 sat
D. Notify the healthcare provider
✅ Correct Answer: C – Apply oxygen and monitor. Airway and oxygen are top priorities in respiratory distress.
Final Thoughts
Respiratory distress in children is a life-threatening condition that requires quick thinking and decisive action from nurses. Whether you’re prepping for the NCLEX, building your nursing bundle study resources, or working bedside as an RN nurse, always stay alert to the signs and ready to intervene.