Reading fetal heart rate (FHR) patterns is a crucial skill for any registered nurse (RN nurse) working in labor and delivery. Properly interpreting these patterns can help you detect fetal distress early and act fast, which is critical both in clinical practice and on the NCLEX. This guide will help you break down decelerations in a clear, simplified way — perfect for your nursing bundle or OB study resources.
🩺 Why Fetal Heart Rate Monitoring Matters
FHR monitoring provides valuable information about how the fetus is tolerating labor. As a nurse, understanding patterns like baseline rate, variability, accelerations, and decelerations can make the difference between a healthy outcome and a crisis.
Continuous electronic fetal monitoring is standard during most deliveries, and you’ll be expected to interpret strips confidently both on the NCLEX and in practice.
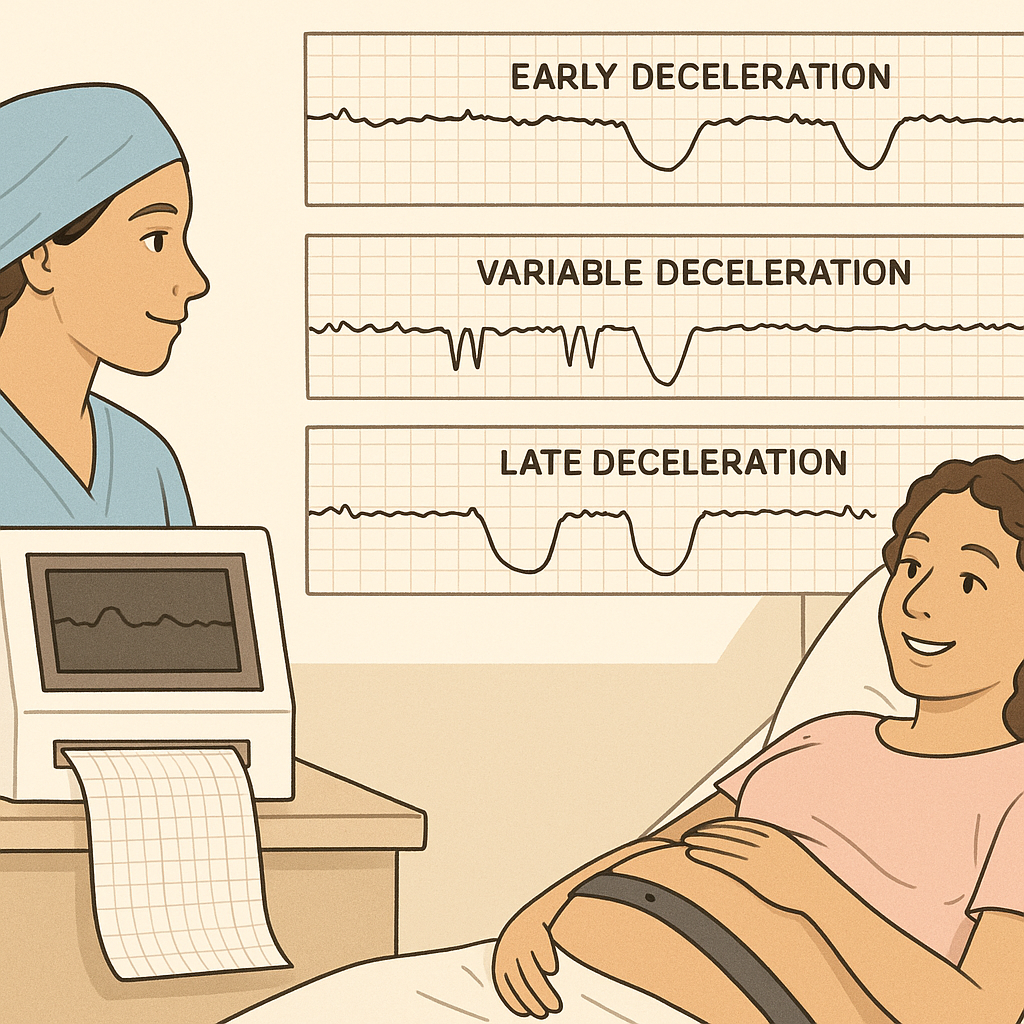
🚼 Types of Decelerations
Decelerations are drops in the fetal heart rate. As an RN nurse, you’ll need to know how to recognize each type and what it means:
1️⃣ Early Decelerations
- Mirror the contraction pattern
- Due to head compression
- Usually benign
- Nursing action: continue to monitor
2️⃣ Variable Decelerations
- Abrupt onset and return
- V- or U-shaped
- Due to cord compression
- Nursing action: reposition mom, check for cord prolapse, give oxygen if needed
3️⃣ Late Decelerations
- Start after contraction begins, recover after contraction ends
- Due to uteroplacental insufficiency
- Most concerning
- Nursing action: reposition mom to left side, give oxygen, stop oxytocin, notify the provider immediately
4️⃣ Prolonged Decelerations
- Last more than 2 minutes but less than 10
- Often caused by cord issues or uterine rupture
- Nursing action: rapid intervention, follow emergency protocols
🧩 Quick Memory Aids for NCLEX
Add these to your nursing bundle:
✅ VEAL CHOP mnemonic:
- V = Variable → C = Cord compression
- E = Early → H = Head compression
- A = Accelerations → O = OK
- L = Late → P = Placental insufficiency
✅ Always assess variability with decels
✅ Remember reposition, oxygen, stop oxytocin for late decels
✅ Know when to call the provider immediately
💡 Other Key Points
- Moderate variability (6–25 bpm) is reassuring
- Absent variability plus recurrent late decels is bad news
- Baseline tachycardia or bradycardia needs evaluation
- FHR below 110 for over 10 minutes = bradycardia
- FHR above 160 for over 10 minutes = tachycardia
As a nurse, you should document:
✅ FHR baseline
✅ Variability
✅ Accelerations
✅ Type, timing, and duration of decelerations
🩹 Priorities for Nurses
When caring for patients with abnormal FHR patterns, remember these steps:
- Continuous assessment
- Timely documentation
- Clear communication with the healthcare team
- Explaining the findings to patients and their families
- Staying calm under pressure
📝 NCLEX Cheat Sheet
✅ VEAL CHOP mnemonic
✅ Decel categories and actions
✅ Baseline and variability norms
✅ Intrauterine resuscitation steps (oxygen, fluids, position change)
✅ Prioritization strategies
Include these in your nursing bundle to master labor and delivery content for the NCLEX.