Heart failure is a common, high-priority topic for every nurse and is guaranteed to appear on the NCLEX. Whether you are a registered nurse (RN nurse) working on a med-surg unit, the ICU, or building your nursing bundle of essential knowledge, understanding heart failure helps you deliver safe and effective patient care.
This guide will break down the pathophysiology, key signs and symptoms, and nursing priorities in simple terms to boost your confidence.
🫀 What Is Heart Failure?
Heart failure happens when the heart can’t pump enough blood to meet the body’s needs. Think of it like a failing pump, causing a backup of fluid and poor tissue perfusion.
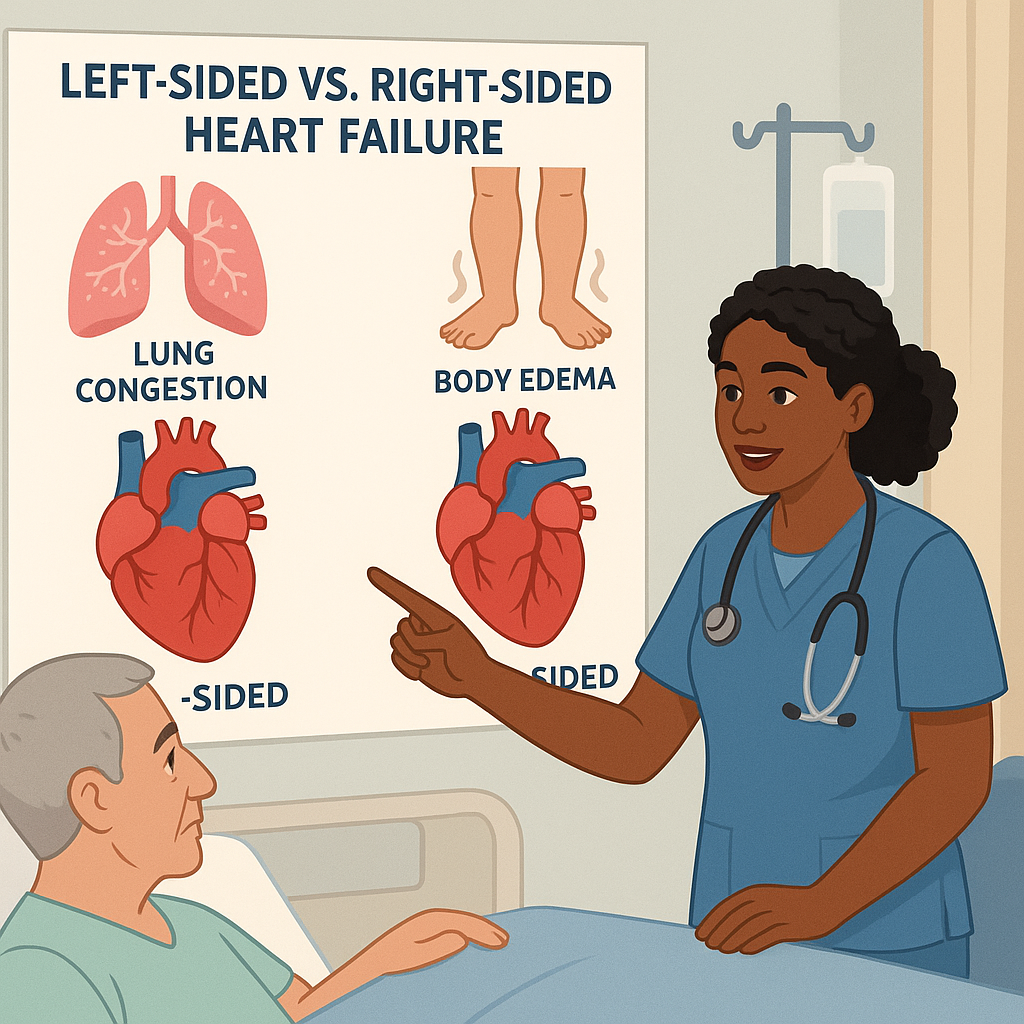
There are two main types:
✅ Left-sided heart failure — the heart cannot pump blood forward to the body, leading to fluid buildup in the lungs (pulmonary congestion).
✅ Right-sided heart failure — the heart cannot pump blood to the lungs, causing fluid to back up in the body (peripheral edema).
Pathophysiology in simple terms:
- Heart muscle becomes weak or stiff
- Fails to fill or empty completely
- Blood backs up
- Fluid leaks into tissues
- Organs don’t get enough oxygen
💡 NCLEX & Nursing Bundle Essentials
The NCLEX loves to test heart failure because of its high prevalence. Every nurse should remember:
- Left-sided failure = L for Lung (crackles, cough, shortness of breath)
- Right-sided failure = R for Rest of the body (edema, weight gain, JVD)
Adding this to your nursing bundle will help you quickly identify priority assessments.
🚨 Key Signs and Symptoms
Left-Sided Heart Failure
✅ Crackles in lungs
✅ Dyspnea on exertion
✅ Orthopnea (trouble breathing lying flat)
✅ Cough, pink frothy sputum (late sign)
✅ Fatigue
Right-Sided Heart Failure
✅ Swelling in legs and feet
✅ Jugular vein distention (JVD)
✅ Ascites (fluid in the belly)
✅ Weight gain
✅ Hepatomegaly (liver enlargement)
🩺 Heart Failure Nursing Priorities
As a registered nurse or future RN nurse, you must act fast to prevent complications. Here’s a simplified priority list:
1️⃣ Assess respiratory status – listen for crackles, monitor oxygen levels
2️⃣ Monitor vital signs – especially heart rate and blood pressure
3️⃣ Daily weights – best indicator of fluid overload
4️⃣ Strict I&O – track fluid intake and output
5️⃣ Positioning – semi-Fowler’s to improve breathing
6️⃣ Administer medications – diuretics, ACE inhibitors, beta-blockers
7️⃣ Patient education – low-sodium diet, medication adherence, daily weights at home
💡 NCLEX tip: If you see pink frothy sputum, that is a sign of pulmonary edema — treat it as a priority emergency!
📦 Add This to Your Nursing Bundle
Don’t forget to include:
✅ Heart failure symptom charts
✅ Medication cheat sheets
✅ Priority nursing interventions checklists
✅ NCLEX practice questions
These resources strengthen your confidence as a nurse and help you pass exams while providing high-quality bedside care.
🧩 Pathophysiology Made Easy
Here’s a quick simplified flow you can memorize:
Heart muscle damage → decreased cardiac output → fluid backs up → organ congestion → poor oxygen delivery
Use this logic on NCLEX questions to understand why your patient develops shortness of breath, edema, or fatigue.
📌 Key Takeaways for Nurses
- Know left-sided vs. right-sided symptoms
- Prioritize breathing, oxygen, and fluid status
- Daily weights are essential
- Teach patients about diet, fluid, and meds
- Add heart failure interventions to your nursing bundle