Accurate pain assessment is one of the most essential skills every nurse must master. Whether you’re preparing for the NCLEX, strengthening your knowledge as a registered nurse, or reviewing materials in your nursing bundle, understanding how to evaluate and document pain properly ensures safe and effective patient care.
🩺 Why Is Pain Assessment Important?
Pain is often called the fifth vital sign because it directly influences healing, sleep, mood, and overall quality of life. Since patients rely on RN nurses to identify and manage their discomfort, accurate assessment and documentation are crucial for guiding treatment decisions.
Furthermore, on the NCLEX, you’ll frequently encounter questions that test your ability to select the appropriate pain assessment tool for specific patient populations.
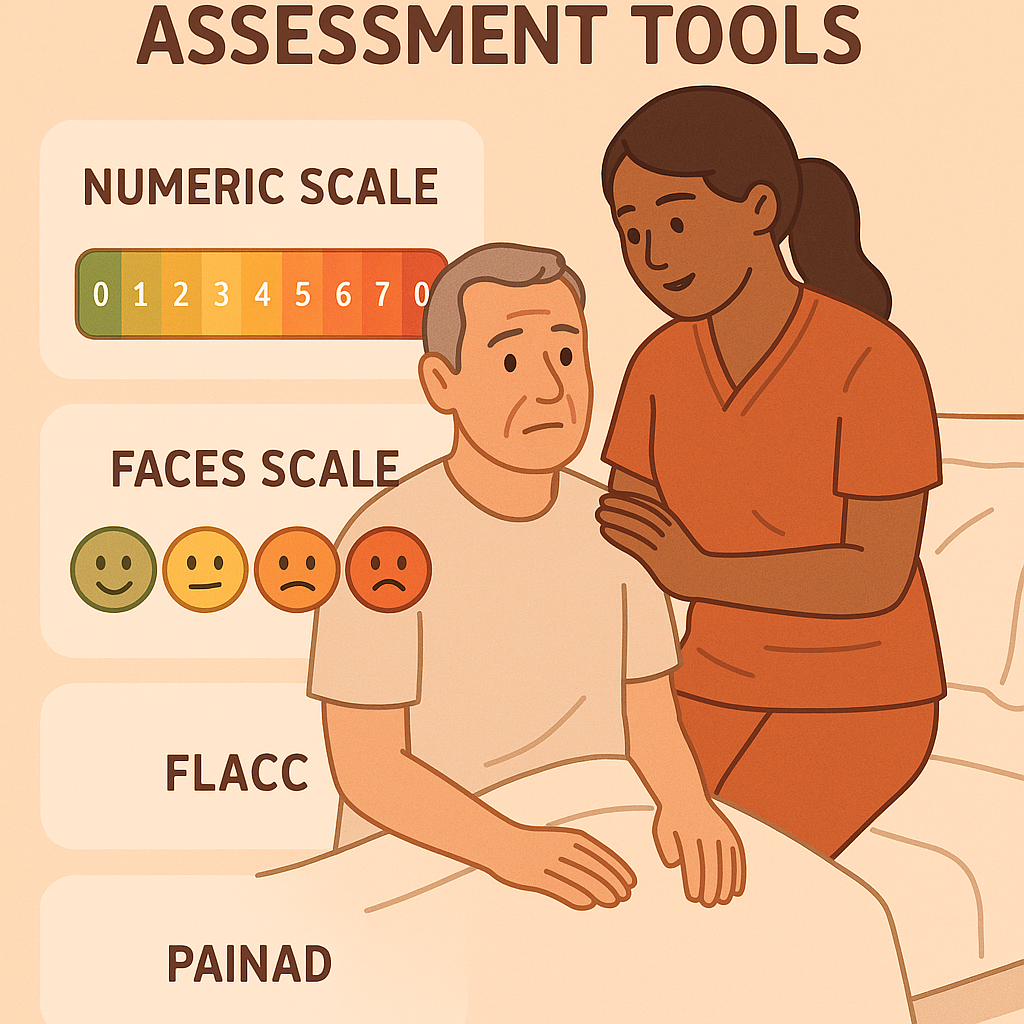
🗂️ Key Pain Assessment Tools for Nurses
Below are the most widely used and tested pain assessment tools that every nurse should know.
1️⃣ Numeric Rating Scale (NRS)
Who it’s for: Most adults and older children capable of clear communication.
✅ Ask:
“On a scale of 0 to 10, where 0 means no pain and 10 represents the worst pain imaginable, what number best describes your pain right now?”
✅ Document:
- The patient’s exact number
- The pain’s location, duration, and aggravating or relieving factors
Using transition phrases such as “in addition” or “furthermore,” nurses should describe any related observations in the patient chart for accuracy.
2️⃣ Visual Analog Scale (VAS)
Who it’s for: Patients who prefer to point or mark pain intensity visually.
✅ How it works:
The patient marks a position on a 10 cm line between “no pain” and “worst pain.”
✅ Nursing tip:
This method is especially helpful for patients who struggle to verbalize pain levels. Moreover, it allows nurses to quickly compare changes in pain intensity over time.
3️⃣ Wong-Baker FACES Pain Scale
Who it’s for: Young children (aged 3 and older) and older adults with communication barriers.
✅ How it works:
Show a set of illustrated faces ranging from happy (no pain) to crying (worst pain). The patient points to the face that best represents how they feel.
✅ NCLEX tip:
This scale frequently appears in pediatric nursing questions. Additionally, it’s a reliable option when assessing non-verbal patients who can still express emotions visually.
4️⃣ FLACC Scale
Who it’s for: Infants, non-verbal patients, or those unable to self-report pain.
✅ What FLACC means:
Face, Legs, Activity, Cry, Consolability — each scored from 0 to 2.
✅ Nursing use:
Add the scores for a total of 0–10. The higher the total, the greater the pain level. Besides, this tool promotes objective assessment when communication isn’t possible.
5️⃣ PAINAD Scale
Who it’s for: Patients with advanced dementia or cognitive impairment.
✅ What it measures:
Breathing, vocalization, facial expression, body language, and consolability.
✅ Nursing note:
It’s particularly useful in hospice or long-term care settings. In addition, consistent use of this scale enhances continuity of care across shifts.
✅ How to Document Pain Like a Pro
Documentation is just as important as the initial assessment. Therefore, every RN nurse should record the following details clearly:
- Pain score (for example, NRS or FLACC number)
- Location — where the pain is felt
- Quality — such as sharp, dull, or throbbing
- Duration — when it started and how long it lasts
- Aggravating and relieving factors
- Response to interventions — Did pain medication help? By how much?
After any intervention, always reassess pain within 30–60 minutes and update the chart. Moreover, communicating pain changes to the healthcare team promotes faster recovery and improved comfort.
🎓 Pain Assessment Tips for NCLEX and Nursing Practice
- Always choose the correct tool based on the patient’s age, condition, and mental status.
- Consistently reassess and document pain before and after interventions.
- Pay attention to non-verbal cues such as grimacing, guarding, or restlessness.
- Additionally, use your nursing bundle practice sheets to review pain scales, case studies, and real-life scenarios.
🗝️ Key Takeaway
A skilled nurse understands that pain is whatever the patient says it is. Through accurate assessment, thorough documentation, and compassionate care, nurses ensure patients receive the relief they deserve while maintaining a safe, professional standard of nursing practice.