Introduction: Why Sinus Rhythms Matter
Especially in critical care and med-surg units, recognizing what’s normal—and what’s not—helps nurses take quick, life-saving actions. Therefore, understanding sinus rhythms is a must for every RN nurse preparing for the NCLEX or working in bedside care.
🫀 What Is a Sinus Rhythm?
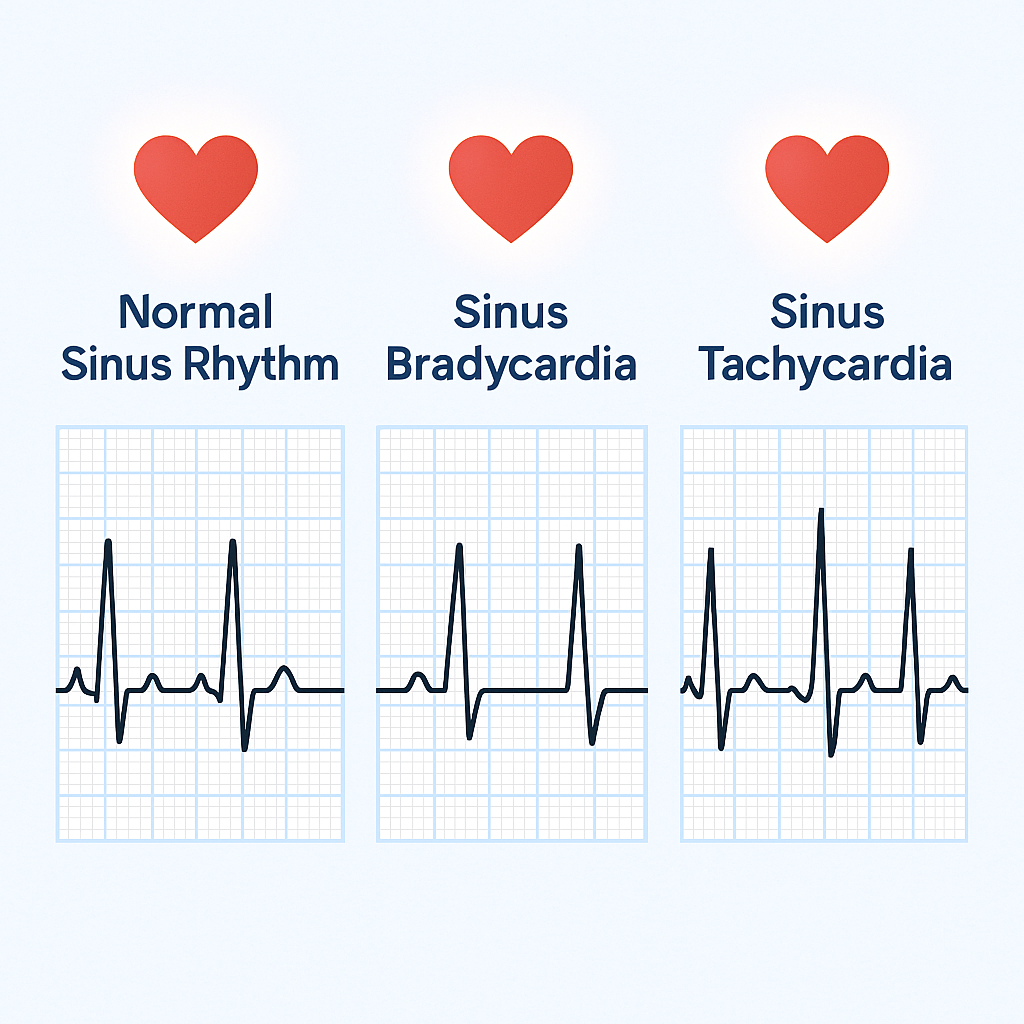
A sinus rhythm means the heartbeat starts in the sinoatrial (SA) node, the heart’s natural pacemaker. In other words, this is what we consider a normal pattern of electrical activity. On an EKG, you’ll typically see:
- A P wave before every QRS complex
- A consistent rhythm
- A heart rate between 60–100 beats per minute
Normal Sinus Rhythm
- Rate: 60–100 bpm
- Rhythm: Regular
- P waves: Present and upright before each QRS
- QRS complex: Normal (0.06–0.10 seconds)
- PR interval: 0.12–0.20 seconds
🧠 What it means: The heart is working as expected. Therefore, no action is needed unless the patient shows symptoms.
❤️ Sinus Bradycardia
- Rate: Less than 60 bpm
- Rhythm: Regular
- P waves: Present before each QRS
- PR and QRS: Normal duration
🔍 Common causes include:
- Athletes (normal finding)
- Vagal stimulation (vomiting, suctioning)
- Medications like beta-blockers or digoxin
- Hypothyroidism
- Increased intracranial pressure
⚠️ Nursing actions:
- First, assess the patient! Are they dizzy, lightheaded, or fainting?
- Then, monitor vital signs closely.
- Moreover, hold medications that slow the heart (if ordered).
- Finally, prepare for atropine or temporary pacing if the patient becomes unstable.
👉 Tip: Sinus bradycardia can be harmless in trained athletes; however, in symptomatic patients, it’s a red flag that requires quick intervention.
❤️ Sinus Tachycardia
- Rate: Over 100 bpm (usually 100–150 bpm)
- Rhythm: Regular
- P waves: Present before each QRS
- PR and QRS: Normal
🔍 Common causes include:
- Fever
- Pain
- Dehydration
- Anxiety or stress
- Shock
- Hypoxia
- Caffeine or stimulant use
⚠️ Nursing actions:
- First, check for symptoms such as chest pain, shortness of breath, or hypotension.
- Then, treat the underlying cause (e.g., give fluids, manage pain, or reduce fever).
- Additionally, monitor for signs of cardiac ischemia in high-risk patients.
👉 In contrast to bradycardia, sinus tachycardia often signals an underlying physiological stressor rather than a conduction problem.
⚡ Quick Tips for Reading Sinus Rhythms on EKG
✅ Use the 6-second strip method: Count the number of R waves in a 6-second strip and multiply by 10.
✅ Always look at the patient, not just the monitor.
✅ Moreover, check the P wave to QRS relationship for consistency.
As a result, these quick checks help prevent misinterpretation during patient emergencies.
🚨 When to Be Concerned
Be alert when you see:
- Sinus bradycardia in a symptomatic patient (dizziness, confusion, low BP)
- Sinus tachycardia with chest pain or signs of decreased cardiac output
- Or, any rhythm that changes suddenly or becomes irregular
Consequently, these findings may indicate a worsening condition that needs rapid nursing intervention.
🩺 Real-Life Nursing Example
Case: A 70-year-old patient shows sinus bradycardia (HR 48 bpm) on telemetry.
➡️ Assessment: He reports dizziness when standing.
➡️ Action: Check BP, hold beta-blocker, and notify the provider. As a result, atropine is ordered to increase the heart rate.
Therefore, this simple assessment prevented a possible syncopal episode.
✅ Conclusion: Master the Basics, Save Lives
Sinus rhythms may seem simple, but they provide vital clues about a patient’s condition. By understanding the differences between normal sinus rhythm, bradycardia, and tachycardia, nurses can respond faster and more effectively at the bedside. Ultimately, mastering these EKG basics doesn’t just help you pass the NCLEX — it helps you save lives every day.