🧠 Why Electrolytes Matter in Nursing
Electrolytes are tiny minerals in the body that carry an electrical charge. They help with:
- Moving fluids in and out of cells
- Sending nerve signals
- Keeping the heart beating
- Supporting muscles and bones
As a nurse, understanding the “Big 4” electrolytes is essential because changes in their levels can be dangerous and life-threatening.
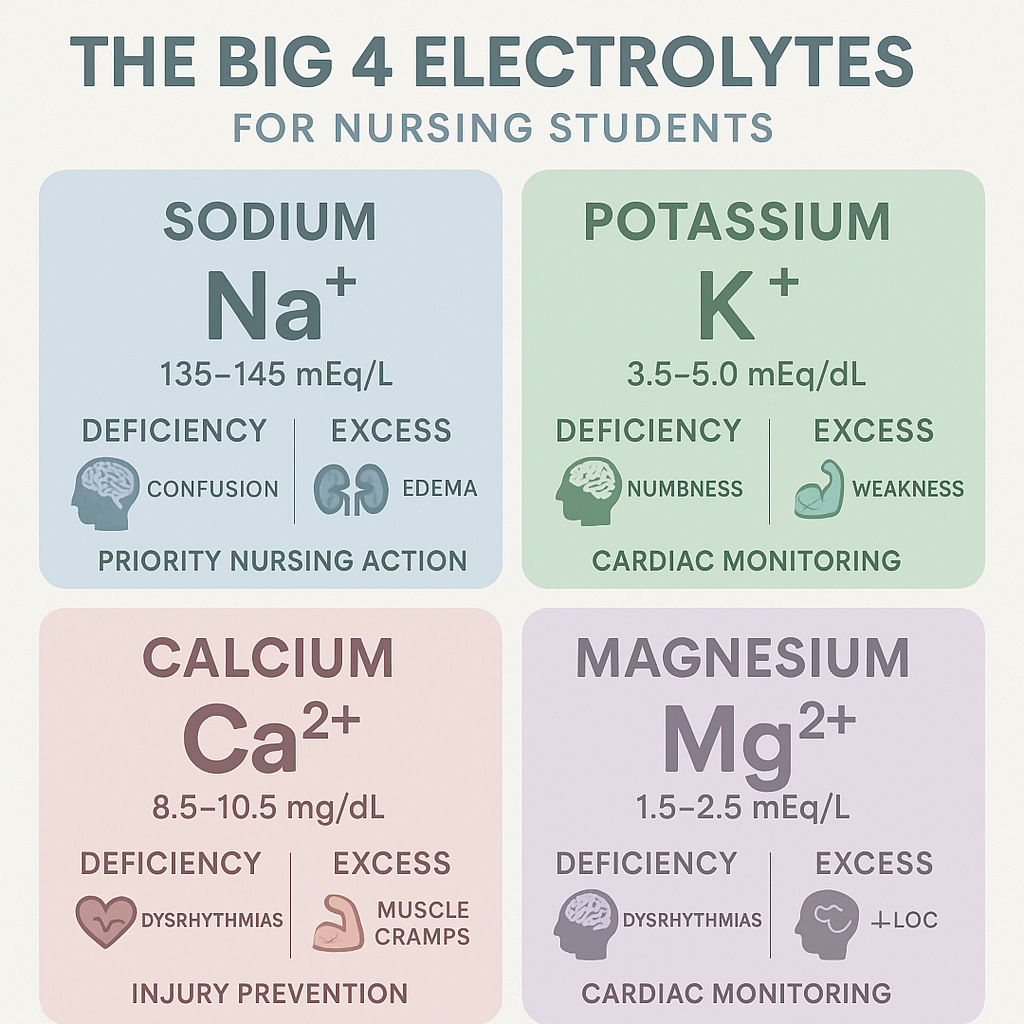
🧂 1. Sodium (Na⁺)
Normal range: 135–145 mEq/L
Main job: Balances water in the body and helps nerve and muscle function.
🔻 Low Sodium – Hyponatremia
Common causes:
- Too much water (dilutes sodium)
- Diuretics (water pills)
- SIADH (a hormone problem)
Signs:
- Headache
- Confusion
- Seizures
- Nausea
What nurses should do:
- Limit water intake
- Monitor mental status
- Administer hypertonic saline (for severe cases)
- Watch labs and vital signs
🔺 High Sodium – Hypernatremia
Common causes:
- Dehydration
- Fever
- Diabetes insipidus
- Not enough water intake
Signs:
- Thirst
- Dry mouth
- Agitation
- Weakness
- Seizures (in serious cases)
Nursing actions:
- Give fluids (oral or IV)
- Monitor input and output
- Protect the brain—do neuro checks often
🍌 2. Potassium (K⁺)
Normal range: 3.5–5.0 mEq/L
Main job: Keeps the heart and muscles working properly.
🔻 Low Potassium – Hypokalemia
Causes:
- Vomiting
- Diarrhea
- Diuretics
- NG suction
- Poor intake
Signs:
- Muscle cramps or weakness
- Constipation
- Flat or inverted T waves on EKG
- Irregular heartbeat
Nursing care:
- Replace potassium (oral or IV carefully)
- Monitor the heart (telemetry)
- Check magnesium—it helps potassium work
Remember: Never give IV potassium fast! It can stop the heart.
🔺 High Potassium – Hyperkalemia
Causes:
- Kidney problems
- Burns or trauma
- Certain medications (like ACE inhibitors)
Signs:
- Peaked T waves
- Muscle weakness
- Slow heartbeat
- Danger: Can cause cardiac arrest
What nurses do:
- Stop potassium intake
- Give calcium gluconate (protects the heart)
- Administer insulin + glucose (pushes K⁺ into cells)
- Consider dialysis if needed
🦴 3. Calcium (Ca²⁺)
Normal range: 8.5–10.5 mg/dL
Main job: Builds strong bones and helps muscles and nerves work.
🔻 Low Calcium – Hypocalcemia
Causes:
- Low vitamin D
- Parathyroid gland issues
- Kidney disease
Signs:
- Muscle twitching
- Numbness in lips or fingers
- Chvostek’s sign (face twitch)
- Trousseau’s sign (wrist spasm when BP cuff inflated)
- Seizures or laryngospasm
Nursing care:
- Give calcium (oral or IV)
- Seizure precautions
- Monitor airway—laryngospasm is a risk
- Encourage foods rich in calcium
🔺 High Calcium – Hypercalcemia
Causes:
- Bone cancer
- Overactive parathyroid
- Too much calcium or vitamin D
Signs:
- Fatigue
- Constipation
- Kidney stones
- Slow reflexes
What nurses do:
- Give fluids to flush calcium
- Loop diuretics
- Monitor the heart
- Educate about avoiding calcium-rich supplements
💪 4. Magnesium (Mg²⁺)
Normal range: 1.6–2.6 mg/dL
Main job: Helps muscles, nerves, and the heart work together. Also works with calcium and potassium.
🔻 Low Magnesium – Hypomagnesemia
Causes:
- Alcoholism
- Malnutrition
- Diarrhea
- Diuretics
Signs:
- Tremors
- Seizures
- Increased reflexes
- Torsades de Pointes (deadly heart rhythm)
Nursing interventions:
- Give IV magnesium sulfate
- Seizure precautions
- Monitor EKG
- Watch deep tendon reflexes
🔺 High Magnesium – Hypermagnesemia
Causes:
- Kidney failure
- Too much magnesium from meds (like antacids or laxatives)
Signs:
- Weakness
- Low reflexes
- Slow heart rate
- Low blood pressure
- Drowsiness
What to do:
- Stop magnesium intake
- Give calcium gluconate (reverses magnesium effects)
- Monitor vital signs closely
- Dialysis if needed
🧾 Electrolyte Quick Chart
ElectrolyteLow Level SignsHigh Level SignsNursing ActionsSodiumConfusion, headache, seizureThirst, dry mouth, agitationLimit fluids, replace Na⁺, neuro checksPotassiumMuscle cramps, flat T wavesPeaked T waves, weak pulseReplace K⁺, insulin/glucose, monitor ECGCalciumTwitching, seizuresFatigue, kidney stonesGive Ca²⁺, hydrate, monitor heartMagnesiumTremors, seizures, TorsadesWeakness, low reflexesIV Mg²⁺ or stop meds, check vitals
🔁 How Electrolytes Work Together
Electrolytes don’t act alone. They affect each other:
- Low magnesium = hard to fix low potassium
- High calcium = low phosphorus
- Sodium levels affect brain cells fast
Always check all electrolyte levels when one is abnormal. And don’t forget about the kidneys—they filter these minerals.
🩺 Nurse Tips for Managing Electrolyte Problems
- Know your labs. Keep a chart of normal values on your phone or clipboard.
- Assess the patient. Don’t treat labs alone. Look for symptoms.
- Use ECG monitoring. Potassium and magnesium affect the heart.
- Go slow with replacements. IV potassium or calcium must be given carefully.
- Educate patients. Teach about foods high or low in specific electrolytes.
- Watch renal function. Kidneys control many electrolytes—if the kidneys fail, so can balance.
🧠 Mnemonics to Remember
- SALT LOSS: Signs of low sodium
- MURDER: Signs of high potassium
- CHvostek’s + TRousseau’s = Ca²⁺ trouble
- MAG = Must Always Guard the heart
🖼️ Visual Learning Tip
Pairing this guide with a visual chart or infographic helps you memorize faster. You can:
- Draw the signs on a diagram of the body
- Use color-coded lab values
- Create flashcards for each electrolyte
📘 Summary
Electrolyte balance is life or death—especially in critical care. As a nurse or student, knowing the Big 4 electrolytes and how to recognize changes will help you:
- Provide faster, safer care
- Spot early warning signs
- Respond with confidence during emergencies