Introduction: Why Magnesium Matters in the ICU
Magnesium is a key electrolyte that plays an essential role in heart function, muscle contractions, and nervous system stability. In the ICU, where patients are critically ill, magnesium levels can quickly fall below normal. This condition—hypomagnesemia—may seem minor, but it can turn life-threatening fast.
In this article, we’ll break down what hypomagnesemia is, what causes it, how to spot it, and why ICU nurses need to act quickly to treat and monitor it.
What Is Hypomagnesemia?
Hypomagnesemia means low levels of magnesium in the blood, typically below 1.6 mg/dL. Magnesium helps with:
- Heart rhythm regulation
- Muscle and nerve function
- Maintaining normal levels of calcium and potassium
- Energy production (ATP function)
When levels drop, serious complications can arise—especially in critically ill patients.
Causes of Hypomagnesemia in ICU Patients
In the ICU, patients often have complex conditions and treatments that increase the risk of magnesium loss. Common causes include:
1. GI Losses
- Chronic diarrhea
- Vomiting
- Nasogastric suction
- Malabsorption disorders (e.g., Crohn’s, celiac disease)
2. Renal Losses
- Diuretics (especially loop diuretics like furosemide)
- Aminoglycosides (e.g., gentamicin)
- Cyclosporine
- Cisplatin (chemotherapy)
3. Alcoholism
Alcohol disrupts magnesium absorption and increases urinary losses.
4. Poor Nutrition or Refeeding Syndrome
Critically ill or malnourished patients may be magnesium deficient, especially during refeeding.
5. Sepsis and Critical Illness
Stress, inflammation, and organ dysfunction can shift magnesium out of cells and increase losses.
Why Is Hypomagnesemia Dangerous in the ICU?
Magnesium is closely linked with heart health, muscle function, and electrolyte balance. Here’s why it’s deadly when it drops:
1. Cardiac Arrhythmias
- Low magnesium increases the risk of ventricular arrhythmias, including torsades de pointes, a dangerous rhythm that can lead to sudden cardiac arrest.
- It worsens hypokalemia and hypocalcemia, both of which also affect heart rhythms.
2. Neuromuscular Complications
- Muscle twitching
- Weakness
- Tremors
- Seizures
3. Electrolyte Imbalance
Magnesium helps regulate potassium and calcium. Without enough magnesium, potassium and calcium corrections won’t work effectively.
4. Refractory Hypokalemia
If a patient’s potassium is low and won’t respond to IV potassium, always check the magnesium.
Signs and Symptoms to Watch For
Hypomagnesemia often goes unnoticed until it causes complications. ICU nurses must know what to look for:
- Muscle cramps or tremors
- Torsades de pointes on EKG
- Positive Chvostek or Trousseau signs (from associated low calcium)
- Irritability, confusion, or seizures
- Frequent PVCs or prolonged QT interval
- Tachycardia
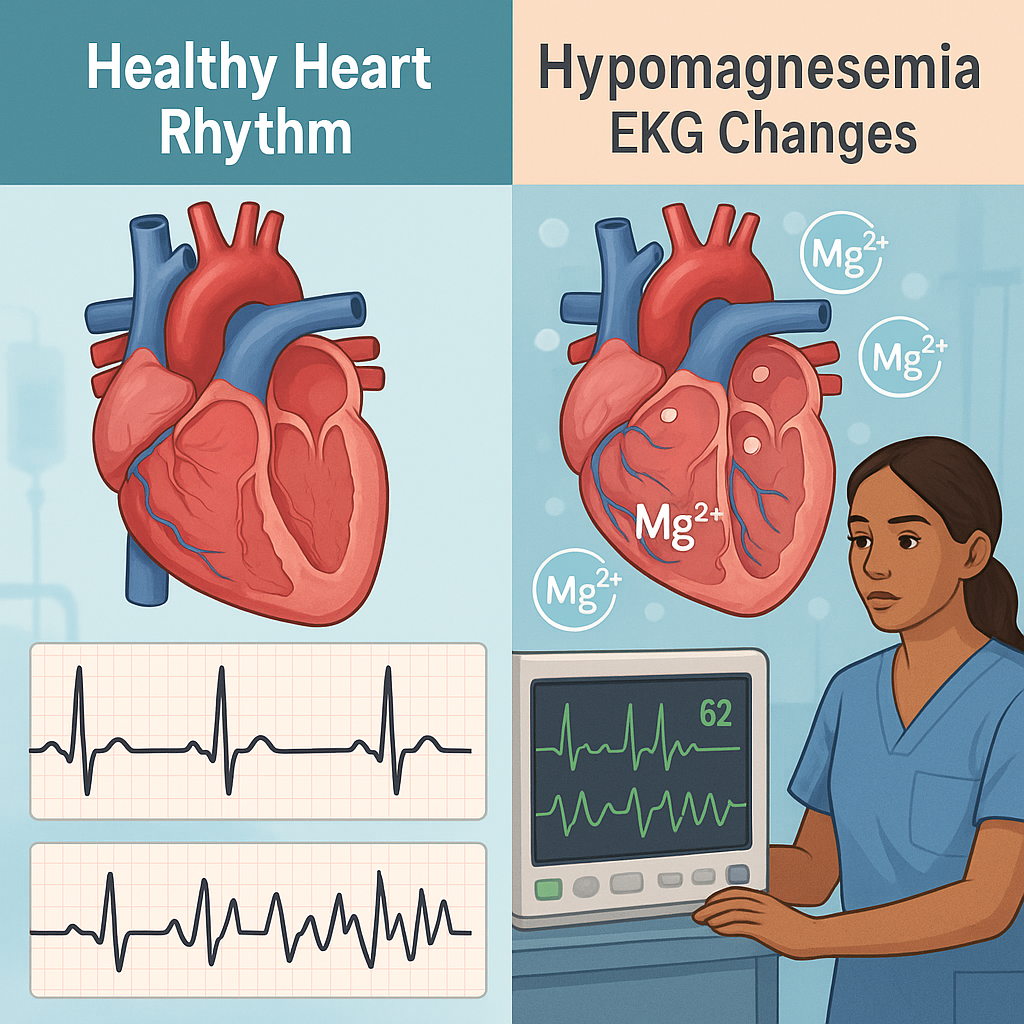
How to Identify Hypomagnesemia on EKG
EKG Clues:
- Prolonged QT interval
- Torsades de pointes (twisting of QRS complexes)
- Frequent premature ventricular contractions (PVCs)
Early recognition of these patterns is critical for preventing cardiac arrest.
Nursing Interventions: What Nurses Must Do
In the ICU, nurses are the first line of defense. Here’s how to act:
1. Assess and Monitor
- Watch for signs: muscle twitching, arrhythmias, altered mental status
- Review labs: magnesium, potassium, calcium
- Monitor EKG for QT changes or new arrhythmias
- Check medication list for drugs causing magnesium loss
2. Replace Magnesium Safely
- Administer IV magnesium sulfate per protocol or provider order
- Infuse slowly: rapid infusion can cause flushing, hypotension, or cardiac arrest
- Monitor deep tendon reflexes and urine output
3. Prevent Further Loss
- Notify the provider if the patient is on loop diuretics or nephrotoxic antibiotics
- Suggest switching to a less magnesium-wasting medication if possible
4. Coordinate with the Team
- Work closely with the provider and pharmacist
- Ensure frequent lab rechecks
- Educate the patient and family about symptoms if appropriate
How Much Magnesium to Give?
Always follow your facility’s protocol. However, a typical ICU order might look like:
- Magnesium sulfate 1-2 grams IV over 1 hour
- Severe cases: up to 4 grams IV slowly
- Maintenance: oral magnesium if GI tract is functioning
Who’s at Highest Risk in the ICU?
- Alcoholics
- Patients with diarrhea or vomiting
- Patients on furosemide or gentamicin
- Sepsis patients
- Burn patients
- Those with uncontrolled diabetes
Be extra alert with these groups and check electrolytes often.
The Link Between Hypomagnesemia and Other Electrolyte Issues
Magnesium doesn’t act alone. Low magnesium often comes with:
- Hypokalemia (low potassium)
- Hypocalcemia (low calcium)
Trying to fix potassium or calcium without correcting magnesium won’t work. Always address magnesium first.
Real-Life ICU Example
Imagine a 68-year-old sepsis patient with a prolonged QT interval and PVCs. Potassium is low (2.9), and the team has been giving KCl with no effect.
You review labs: magnesium is 0.9 mg/dL—very low.
You alert the provider, start IV magnesium, and within an hour, the rhythm stabilizes, and potassium levels start to rise.
This is a real, life-saving moment—and it’s why ICU nurses must never ignore magnesium.
Preventing Hypomagnesemia in ICU Patients
Prevention is just as important as treatment:
- Routine magnesium checks in high-risk patients
- Avoid unnecessary diuretics
- Early replacement in patients on antibiotics like gentamicin or amphotericin B
- Use magnesium-containing enteral feeds if tolerated
- Educate your team on the importance of magnesium balance