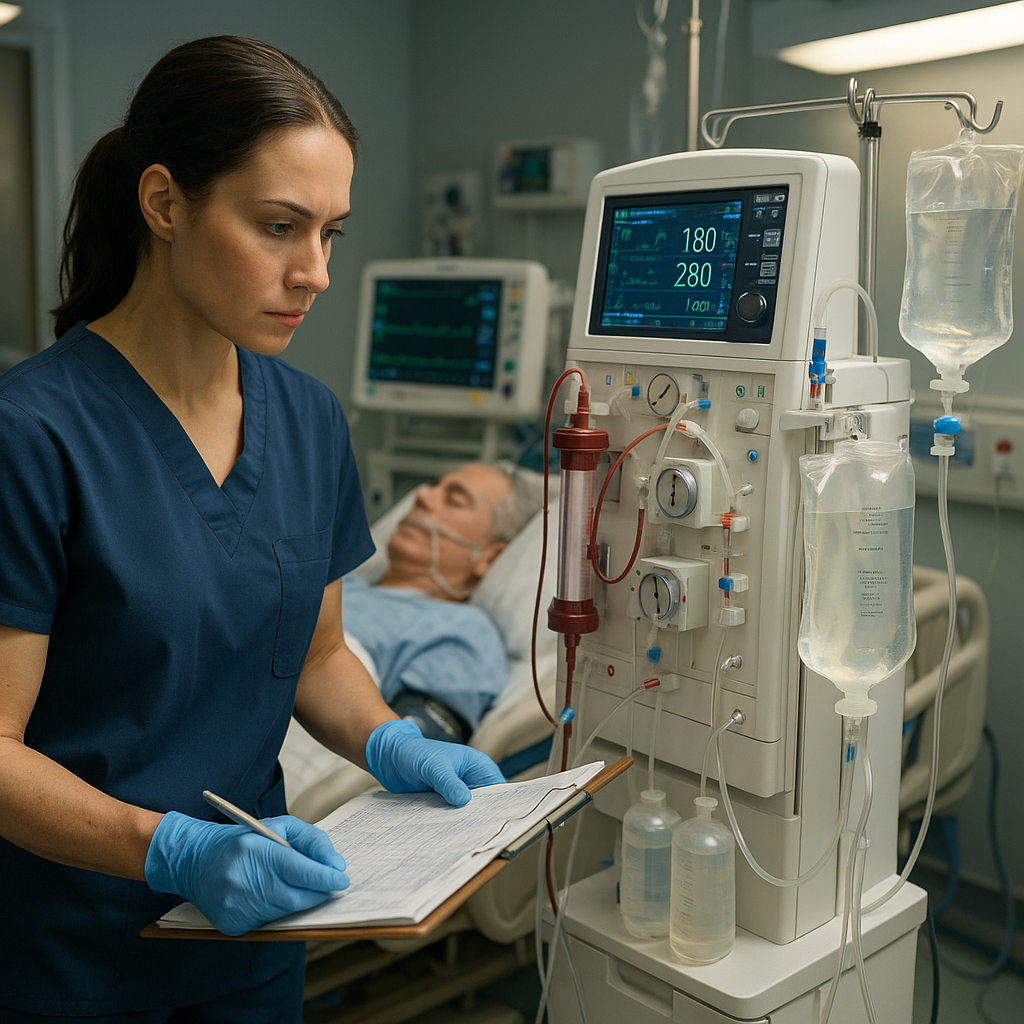
Continuous Renal Replacement Therapy (CRRT) is commonly used in intensive care units to support patients with acute kidney injury (AKI) or fluid overload who are too unstable for traditional dialysis. For ICU nurses, understanding how CRRT works and knowing what to monitor is essential for patient safety and successful treatment.
What is CRRT?
CRRT is a slow and continuous form of dialysis that filters the blood over 24 hours. Unlike hemodialysis, it avoids large fluid shifts and is better suited for unstable, critically ill patients.
This therapy helps:
- Remove waste products (urea, creatinine)
- Control electrolytes (potassium, sodium)
- Balance fluids
- Manage acid-base disturbances
Why CRRT is Used in the ICU
Patients in the ICU often face multiple organ failures. CRRT helps manage:
- Acute Kidney Injury (AKI)
- Sepsis-induced renal failure
- Severe fluid overload
- Drug overdoses or toxin removal
What ICU Nurses Need to Monitor During CRRT
1. Access Site
- Check the central venous catheter (usually in the internal jugular or femoral vein) for signs of bleeding, infection, or dislodgement.
- Maintain aseptic technique during dressing changes.
2. Filter Function
- Monitor for clotting of the filter.
- Observe pressure readings: transmembrane pressure (TMP) and access pressures. A rising TMP may signal clotting.
- Replace the circuit if alarms indicate decreased flow.
3. Fluid Balance
- CRRT machines remove fluid continuously. Nurses must track:
- Total fluid input and output
- Net fluid balance every hour
- Sudden drops in blood pressure (may signal excessive fluid removal)
4. Electrolytes and Labs
Frequent labs help adjust therapy:
- Potassium: Watch for hypokalemia.
- Calcium & Magnesium: Can decrease with citrate anticoagulation.
- Phosphate: Often needs supplementation.
- BUN and Creatinine: Evaluate effectiveness of therapy.
5. Anticoagulation
- Heparin or citrate is often used to prevent filter clotting.
- Monitor:
- aPTT if using heparin
- Ionized calcium levels if using citrate
- Bleeding signs
6. Hemodynamic Status
CRRT can affect blood pressure.
- Monitor for hypotension.
- Collaborate with the medical team to adjust fluid removal rates.
- Use vasopressors if needed to maintain perfusion.
7. Machine Settings
Know how to:
- Adjust fluid removal goals
- Pause or restart the machine
- Respond to alarms quickly and safely
Nursing Responsibilities in CRRT
- Educate the patient and their families about the process.
- Communicate with nephrology, ICU providers, and pharmacists.
- Document machine settings, vital signs, lab values, and patient responses.
- Troubleshoot alarms and recognize complications early.
Common Challenges for Nurses
- Filter clotting or machine downtime
- Managing sudden lab abnormalities
- Keeping up with frequent lab draws and fluid adjustments
- Maintaining sterile technique under pressure
Tips for Success
- Stay up to date with hospital protocols and training.
- Double-check orders for dialysate and replacement fluids.
- Communicate hourly I&Os clearly to the ICU team.
- Report early signs of complications.
Conclusion
Renal Replacement Therapy is complex, but with the right knowledge and monitoring, nurses can ensure safe and effective care for ICU patients. Staying alert to changes in fluid status, labs, and filter performance is key. CRRT isn’t just a machine process—it’s a nursing priority.