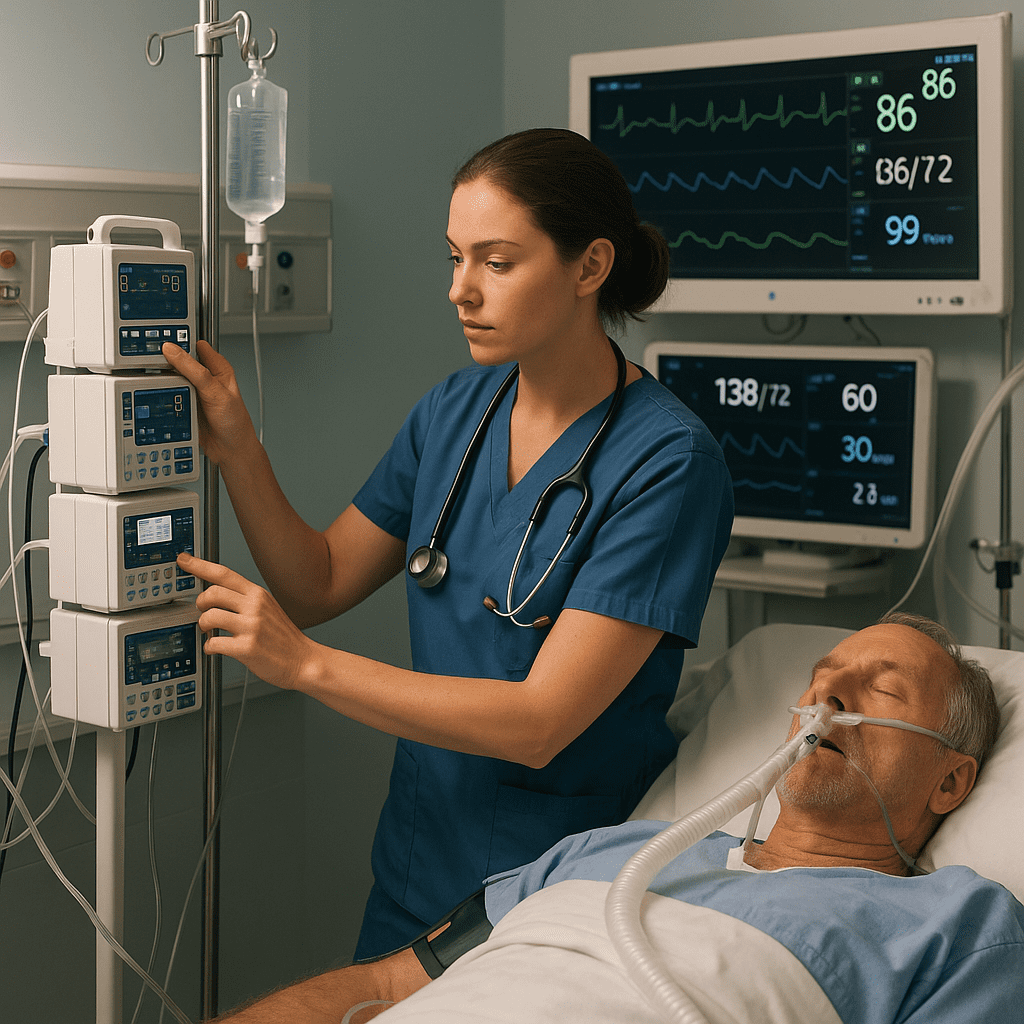
Critical care nursing requires more than just compassion — it demands precision, vigilance, and a deep understanding of the medications that keep patients alive. In the Intensive Care Unit (ICU), continuous IV drips (infusions) are used to maintain blood pressure, manage pain, and ensure patient comfort during life-threatening conditions.
This guide simplifies the most important ICU drips — vasopressors, sedatives, and analgesics — in a way that every nursing student, RN nurse, or registered nurse preparing for the NCLEX can easily understand.
💉 What Are ICU Drips?
ICU drips are continuous intravenous (IV) infusions that deliver medications in a steady, controlled manner. Unlike bolus doses, these drips allow nurses to adjust the rate depending on the patient’s response.
These drips are often life-saving, especially for patients with:
- Shock (septic, cardiogenic, or hypovolemic)
- Mechanical ventilation requiring sedation
- Severe pain or post-operative conditions
As a critical care nurse, knowing the purpose, mechanism, and nursing implications of each drip is essential for safe practice and NCLEX success.
⚡ 1. Vasopressors — The Blood Pressure Lifesavers
🧠 What Are Vasopressors?
Vasopressors are medications that constrict blood vessels and raise blood pressure. They are used when a patient’s mean arterial pressure (MAP) drops dangerously low — commonly seen in septic shock or cardiac arrest.
These drugs act on alpha and beta receptors in the body to restore tissue perfusion and maintain organ function.
💊 Common Vasopressors Used in the ICU
| Medication | Mechanism | Key Nursing Points |
|---|---|---|
| Norepinephrine (Levophed) | Alpha and beta-adrenergic agonist — increases BP by vasoconstriction | – First-line for septic shock – Monitor MAP ≥ 65 mmHg – Must run through central line |
| Epinephrine (Adrenaline) | Stimulates alpha and beta receptors | – Used for anaphylaxis and cardiac arrest – Watch for tachycardia and dysrhythmias |
| Dopamine | Dose-dependent effects: low = renal, high = vasoconstriction | – Monitor urine output – Risk of tachyarrhythmias |
| Phenylephrine (Neo-Synephrine) | Pure alpha agonist | – Increases BP without affecting heart rate – Useful when tachycardia is a concern |
| Vasopressin | Acts on vasopressin receptors for vasoconstriction | – Often added to norepinephrine – Do not titrate independently |
🩺 Nursing Responsibilities for Vasopressors
As a registered nurse, you play a critical role in titrating and monitoring vasopressors safely.
Nursing considerations:
- Always use a central line (to prevent extravasation injury).
- Monitor blood pressure every 2–5 minutes during titration.
- Assess extremity perfusion (cool or mottled skin = poor perfusion).
- Monitor urine output and lactate levels for tissue perfusion.
- Taper off slowly — sudden discontinuation can cause hypotension.
💡 NCLEX Tip:
If a patient on norepinephrine has a MAP below 65 mmHg, the nurse’s priority is to titrate the drip upward per protocol — not to stop it or give a fluid bolus unless ordered.
💤 2. Sedatives — Keeping Patients Calm and Safe
🧠 Why Sedation Is Used in the ICU
Sedation helps mechanically ventilated patients remain comfortable and reduces anxiety, agitation, and oxygen consumption. It also ensures safety during invasive procedures like intubation or central line insertion.
For the nurse, maintaining the right sedation depth is essential — too little causes agitation, too much leads to hypotension and prolonged ventilation.
💊 Common ICU Sedatives
| Medication | Mechanism | Key Nursing Points |
|---|---|---|
| Propofol (Diprivan) | Enhances GABA activity (CNS depressant) | – Rapid onset, short duration – Causes hypotension & bradycardia – Check triglycerides daily (risk of Propofol Infusion Syndrome) |
| Midazolam (Versed) | Benzodiazepine — increases GABA | – Provides amnesia & anxiolysis – Risk of respiratory depression – Antidote: Flumazenil |
| Dexmedetomidine (Precedex) | Alpha-2 agonist for light sedation | – Less respiratory depression – Common for weaning ventilated patients – May cause bradycardia |
| Lorazepam (Ativan) | Benzodiazepine — long-acting | – Used for continuous sedation or status epilepticus – Watch for propylene glycol toxicity |
🩺 Nursing Responsibilities for Sedatives
As an RN nurse, your role is to ensure patient comfort while avoiding oversedation.
Nursing considerations:
- Assess RASS (Richmond Agitation-Sedation Scale) every hour.
- Monitor airway, respiratory rate, and SpO₂ continuously.
- Check blood pressure and heart rate closely.
- Provide daily sedation vacations (unless contraindicated).
- Ensure the patient is pain-free before reducing sedation.
💡 NCLEX Tip:
If a sedated patient becomes hypotensive, decrease or stop the propofol drip first — then notify the provider.
💊 3. Analgesics — Managing ICU Pain Effectively
🧠 Why Pain Control Matters in Critical Care
Pain in the ICU is often underrecognized. Patients on ventilators or post-surgery cannot always express pain verbally. Effective pain management reduces stress, improves outcomes, and helps stabilize vital signs.
For every nurse, pain assessment and management are a top nursing priority — both in real-life ICU care and on the NCLEX exam.
💊 Common Analgesic Drips in the ICU
| Medication | Mechanism | Key Nursing Points |
|---|---|---|
| Fentanyl | Potent opioid agonist | – Fast onset and short duration – Ideal for mechanically ventilated patients – Monitor for respiratory depression |
| Morphine | Opioid agonist | – Provides long-lasting pain relief – Can cause hypotension and histamine release |
| Hydromorphone (Dilaudid) | Strong opioid, more potent than morphine | – Watch for sedation and bradypnea – Adjust dose for renal impairment |
| Ketamine | NMDA antagonist — provides pain relief and sedation | – Maintains airway reflexes – May cause hallucinations or increased ICP |
🩺 Nursing Responsibilities for Analgesics
Nurses are responsible for balancing pain relief with patient safety.
Nursing considerations:
- Use pain scales (CPOT for non-verbal patients).
- Monitor vital signs and level of consciousness.
- Assess for respiratory depression or hypotension.
- Taper opioids slowly to prevent withdrawal symptoms.
- Document pain reassessments and patient response accurately.
💡 NCLEX Tip:
If a patient on a fentanyl drip becomes unresponsive with a low respiratory rate, the nurse should stop the infusion and administer naloxone (Narcan) per protocol.
🧠 Integrating ICU Drips into NCLEX Nursing Practice
Understanding ICU drips goes beyond memorization — it’s about critical thinking, safe administration, and prioritization. The NCLEX tests your ability to apply pharmacology concepts in emergency and ICU settings.
Here’s how this topic ties into NCLEX nursing questions:
- Priority questions: What to do when BP drops on a vasopressor
- Pharmacology: Recognizing side effects and antidotes
- Delegation: Which tasks can be assigned to an LPN or UAP
- Safety: When to hold or adjust continuous infusions
For nursing students and registered nurses reviewing this topic, using a Nursing Bundle that covers Critical Care, Pharmacology, and Medical-Surgical Nursing helps reinforce concepts through visuals, cheat sheets, and step-by-step explanations.
📘 Summary Table — ICU Drips at a Glance
| Category | Example Medications | Key Nursing Focus |
|---|---|---|
| Vasopressors | Norepinephrine, Epinephrine, Vasopressin | Maintain BP and perfusion |
| Sedatives | Propofol, Midazolam, Dexmedetomidine | Monitor RASS, airway, and hemodynamics |
| Analgesics | Fentanyl, Morphine, Ketamine | Control pain, prevent respiratory depression |
💬 Final Thoughts for the RN Nurse
Working in the ICU is one of the most demanding yet rewarding areas of nursing. Every registered nurse must understand how ICU drips affect patient outcomes — when to titrate, when to stop, and when to act fast.
If you’re preparing for the NCLEX or just starting your critical care nursing journey, focus on learning these drips step by step. Use tools like the Critical Care Nursing Bundle or Pharmacology Nursing Bundle to reinforce your knowledge with real-life examples and simplified guides.
Remember — in the ICU, your attention to detail can save a life. 💙
❓FAQs: ICU Drips for Nurses and NCLEX
Vasopressors raise blood pressure.
Sedatives keep patients calm or unconscious.
Analgesics relieve pain.
Each has specific monitoring parameters every nurse must know.
Norepinephrine (Levophed) is the first-line choice. It’s a favorite NCLEX question and critical for every RN nurse to memorize.
Because it can cause severe hypotension, bradycardia, and Propofol Infusion Syndrome if used long-term or at high doses.
Maintaining adequate perfusion and blood pressure while preventing extravasation injuries.
By studying through NCLEX-focused nursing bundles, which break down each medication into easy charts, side effects, and nursing tips for quick recall and safe practice.